Does Diet Influence the Risk of Developing Rheumatoid Arthritis (RA)?
“The Mediterranean diet, rich in fish, plant food, mono- and polyunsaturated fat, and including moderate wine consumption, has been suggested to protect against e.g. cardiovascular disease, but its effect on RA development has only been studied to a limited extent.”[1]
Do Mediterranean or vegetarian diets impact Rheumatoid Arthritis risk?
 The Swedish Epidemiological Investigation of Rheumatoid Arthritis (EIRA) enrolled 1296 people diagnosed with rheumatoid arthritis between 2005 and 2012. People with rheumatoid disease (PRD) were compared with 2661 randomly selected controls matched by age, sex and residential area.
The Swedish Epidemiological Investigation of Rheumatoid Arthritis (EIRA) enrolled 1296 people diagnosed with rheumatoid arthritis between 2005 and 2012. People with rheumatoid disease (PRD) were compared with 2661 randomly selected controls matched by age, sex and residential area.
People who had been diagnosed with RA were asked about the food they ate during the year before being enrolled in the study, including Western diet, Mediterranean diet, vegetarian diet, vegan diet, or other specific diet. “9% of the RA-cases (n=122/1296) reported to consume a Mediterranean diet the year before enrolment compared with 12% (309/2661) of the controls, and 4% (n=47/1296) of the RA cases and 3% (80/2661) of the controls reported to consume a vegetarian diet.”
Diet and lifestyle questions need to be studied
Questions of diet and lifestyle are often tangled in controversy when considered in the context of chronic disease. The onus is often placed on individuals to prevent developing chronic diseases that increase healthcare costs. However, “common sense” does not always parallel scientific evidence; we must ask even the questions we consider “obvious” and examine evidence objectively.
Findings related to the risk of developing rheumatoid disease and diet
Here’s what the study concluded:
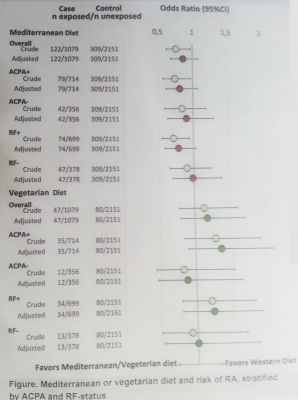
1) PRD who said they consumed a Mediterranean diet had a lower risk of being diagnosed with RA in an unadjusted analysis. However this association disappeared after adjustment for potential confounding factors such as body mass index, smoking, formal education, and physical activity.
2) PRD who were ACPA (anti-CCP) positive or rheumatoid factor positive had a tendency toward lower risk with a Mediterranean diet.
3) There was no relationship found with PRD who consumed a vegetarian diet.
What caused the small difference in people who were antibody positive? Were there other differences at their disease onset?
What about you?
Some who have been diagnosed with RD fit a profile that is considered typical; and others of us developed the disease despite the lack of what are sometimes considered risk factors. Personally, I should’ve been safe from RD since nursing babies is considered protective from it[2]… Exercised, never smoked, and ate a healthy diet. What about you? Do you think diet or another factor impacted whether you developed rheumatoid disease?
FOOTNOTES
[1] Johansson K, Sandberg M, Saevarsdottir S, Neovius M, Alfredsson L, Askling J, Bengtsson C. Do Mediterranean or Vegetarian Diets Influence the Risk of Rheumatoid Arthritis? Arthritis Rheum Abstract Supplement [Internet]. 2014 Nov 16 [cited 2014 Nov 23]: Abstract #2018. Available from http://www.acrannualmeeting.org/wp-content/uploads/2014/10/2014-ACR_ARHP-Annual-Meeting-Abstract-Supplement2.pdf
[2] Pikwer M, Bergstrom U, Nilsson JA, Jacobsson L, Berglund G, Turesson C: Breast feeding, but not use of oral contraceptives, is associated with a reduced risk of rheumatoid arthritis. Ann Rheum Dis [Internet]. 2009 Apr [cited 2014 Nov 23]:68;4:526-530. Abstract available from http://www.ncbi.nlm.nih.gov/pubmed/18477739
Related stories
Modeled after Food Network’s Hell’s Kitchen, the original RA Kitchen project started because “we need easier –FASTER – recipes. We often need different tools. We need ideas for getting more of those certain ingredients into our food: Omega 3’s, anti-oxidants, and vitamins to fight infection…” Click to continue reading Rheumatoid Arthritis and the Kitchen: Hey, We All Eat!
Cigarette smoke and other toxins contribute to the risk of RD. Smoking is one of the few risk factors that emerges consistently in studies of rheumatoid disease, and has led to the study of other environmental risks. Specific studies are beginning to untangle the risks from the myths of What Causes Rheumatoid Arthritis Disease to Trigger? Read more on Smoking and Rheumatoid Arthritis: 6 Things You Need to Know.




I nursed my babies for a total of four years. We exercised, walked miles a day, my entire family ate wholesome foods, whole grains, numerous vegetables, all home cooked meals, rarely ate sugar, ate primarily low fat, I made our breads and cereals, we grew many of our own veges, didn’t smoke, rarely drank and when we did it was wine. I have significant RA as did my mother. I am serum negative and all my tests are negative. The only evidence of extensive RA is the significant bone erosion seen on my Xray and nuclear scans along with swelling and pain. I take studies with a grain of salt. They seem so often to be trying to justify a way to blame the victim; in this case for having not eaten something or eating the wrong something.
Absolutely. I think RD ‘hit’ at the time it did because of excessive stressors in our household. I was burdened with too much responsibility and then defending a frivolous lawsuit against my husband and his father’s estate. I did a lot of research for the lawsuit, but at the two year mark I remember telling my husband something catastrophic was going to happen to me (because I felt so horrible all the time). Three months later it hit. Being an athlete, I thought it was a pulled muscle, but within two weeks the pain and inability to move had spread throughout my body. The diagnosis came.
I do believe the level of the continuous stress/tension experienced during that time impacted the onset of RD.
Hi Kelly!
This topic about diet and the potential impact on RD has been something I’ve been questioning for quite awhile now. Review of my risk factors and protective behaviors. After my second marriage in 2008, I followed a vegetarian diet with my husband but I had joint symptoms that started in 2005 but didn’t consider DX of RD at that time. From 2005-present with increasing number of joints involved it significantly impacted my activity that I gained weight. Exercised my whole life been very very active until this stage in my life. Menopause also occurred during this time frame. So I had weight gain… the most I’ve ever gained in my life 35ibs! Struggling to get it off! I’ve never smoked ever but exposed to second hand smoke as a child until I moved away from home. I wonder if second hand smoke can still increase ones risk?? Like you I nursed my 3 children. I do have family history of RD but somewhat distant (great aunt and uncles) on both sides. My father had arthritis assumed it was osteo but he had problems with his feet just like mine. He’s deceased so won’t ever know for sure. Fast forward, changed my diet to Weston A. Price diet as much as possible past 18 months fresh, organic, local, return to pastured animal fats, cod liver oil, etc. prepare most of my food at home. I still limit meat and eat more fish. Finally a Rheum DX me with inflammatory arthritis in Oct this year calling it rheumatoid but I have no positive blood markers. Bone scan helped make DX. She also DX me with Hashimoto’s although I’ve been DX as hypothyroid for over 10yrs. Previous
PCPs never checked for Hashimoto’s. So, I feel like I’ve done many things right lifestyle wise but didn’t seem to matter. I’ve just started treatment and have so far pretty good response ( hasn’t stopped all my symptoms but they’re improved) to methotrexate with minimal side effects. I do wonder if dietary measures can decrease symptoms or help slow progression.
Thank you for all your research and your website. I can’t tell you how tremendously helpful your site is and it helped me pull together all the “weird symptoms” I’d been experiencing over the past 9 years.
Susan
hi kelly.
this matter of western versus asian or mediteranean diet is so fraught with wrong headednes.
what is a western diet? i was stunned several times now firtsby Asians ans later by southamemricans and then again by east European immigrants. so many think that the “American”Diet is a nonstop engorgement of pizza, hot-dogs, cold-cuts, sugar box cereal, chips, pop, desserts, etc. their reference point until they get to know a wide variety of americans is limited to commercials and TV. i sometimes think people who should know better confuse “Western Diet” with “out of a bag or box diet.” i had all of the above and served my kids these things, on a limited basis. you know the hurry up no time, energy or the special occasion thing.
Our western diet, included veggies; fresh, frozen or canned depending on availability and money. It included rice or pasta or potatoes (not all 3 on same meal. oatmeal was the staple breakfast more than 60% of our year. and so one. so No; a poor quality diet will catch up with you and even exaggerate health problems;– but– an excellent diet and healthful lifestyle does not prevent RD.
My RD was a sneaky unidentified shadow most of my life. I did not know there was something physically wrong with me. i thought i was a”failure” because i would have to step back and guard my “tiredness”. I was reasonably active, never smoke, rarely drank, all the right things.
My RD became full blown and has left my operating on very flat tires after a long period of incredible stress. I do identify with Donna about “excessive stressors”.
so much time and money being wasted on diet studies. i wish there were serious studies on real stress and health.
my maternal grandmother died of age and Rheumatoid complications several years before mom married. living relatives have no clear recollections of her having health problems prior to a violent onslaught of RD that left her apartment bound and latter bed bound.
BUT STRESS , yes that was an issue. she had 6 sons of age at the beginning of WWII. 5 were in the militarily. from what people say she was a pillar of strength and humor (despite burying a daughter) during that time. 2 months after her last son returned from war she collapsed in horrid pain. the pain toned down, never left and she never managed stairs again. In the end she was spoon fed and carried to the bathroom. no way a poor girl from Ireland, later raising a large brood during the depression etc ever squandered $$ on junk foods, sweets or a lascivious lifestyle.
Kelly i am glad you are back and hope that you and your family are kept close to your Lord. I do not know much of your personal life but the bits you reference. –not my business. but i do know your plate seems very full. I hpe your time away was restorative to soul and body. —bye now
Hi Kelly So glad to see your posts again!
I appreciate this article, and wish to mentioned (like others) I am frustrated that my illness is not understood better and I do not like being held responsible for it, based on my diet, lifestyle or anything.
I do wonder if what I eat in any given day adds to or increases my pain and inflammation? I am yet, after 4 years diagnosed, to see any direct correlation, honestly I wish there was, anything to have even an once of control would be nice.
Best Amy
Like Amy, I’ve grown tired of remarks made by seemingly intelligent individuals insinuating something I might eat or drink or not eat or drink would dramatically have an effect on this disease. Yesterday my dentist said, “There are many things that influence inflammation in the body. One food that reduces it is cinnamon.” He looked at me like I have some control over this! I’ve eaten cinnamon all my life. I was just speechless, but I’m TIRED of being spoken to as if ‘I’ in some way caused my RA. I wish I had a polite, yet effective reply to these comments that they would remember. Anyone?
AMEN, Karen. Not sure if there might be something here to help with that https://www.rawarrior.com/20-replies-to-things-not-to-say-to-a-rheumatoid-patient/
I do believe diet influences rd. For me I feel like it’s too late. My fate is sealed. Was dx at 8 yrs old. I believe the damage is done and I can’t go back. Thanks Kelly
i believe that diet may make your symptoms better or worse. As with over eating or not eating enough, we know how this makes us feel. With this disease certain ways we eat and what we eat will aggravate or make our symptoms better. As of the disease, I believe it is all in our dna. It is in my family but may not be in someone else’s. I believe that stress is a big component in this disease. Most individuals who have this disease are not the classic “textbook” case. We are all individuals and how a disease acts with each of us is not necessarily textbook but unique. Unfortunately most of us are treated as textbook cases. My mom had it I have it my youngest daughter has it and possibly another daughter. We all “came down” with RD at different times in our lives. What triggered it, who knows! But I believe it is in our genes.
The 2 years prior to my dx I was the healthiest I have ever been. I was working out 5 times a week and eating a very good diet of organic meats and tons of veggies. I breast fed both my kids and my family has no history of RD. Never smoked a day in my life and drank very little. When my RD kicked in I had HUGE stress…my marriage was breaking down and my kids were not dealing with things well at all, one had to be hospitalized for depression.
Fast forward 2 years and I am free of the marriage stress, kids are healthy and happy and I am symptom free! My doc has suggested cutting back to yearly visits and a possible reduction in meds after my next appointment. For me, I think that stress was the factor that kick started my RD. I don’t feel that my diet or exercise contributed at all.
At 48 I was perfectly healthy, and no one in my family had ever heard of RD. I believe the stress of my divorce, losing my home, and being a single mom is what did me in. My rheumatologist said that it may very well have been an underlying condition I had before but the stress or menopause changes brought it out.
I have been basically vegetarian since my teens, occasional seafood. None of my three children ever even once used a bottle- breastfed all the way. I walk a mile to and from work each day, another mile or so in the evening with the dog. Drink sparingly,have dessert here and there, no fast food.
No, I don’t think diet causes this. Americans have a bizarre relationship with food. We’re forever trying to use food as medicine, which it is not. It’s fuel, and in many cultures, a source of identity and an occasion to sit with family and friends to recharge the soul as well as the body.
My theory is that all the gluten-free, Paleo, whatever, is an unconscious attempt to deal with the huge array of fresh, beautiful foods available to us. People don’t trust themselves to decide what to have for lunch so look for a set of rules (and a rationale, however absurd) to justify their choices.
As others have said, blaming diet for illness also gives folks a great chance to, indirectly or not, blame the victim while assuring themselves that they will never ever ever get sick because they drink gluten-free bottled water.
I,like others believe stress brought mine on, maybe not the cause, but definitely brought it on. For me, a sudden diet change to gluten free did temporarily relieve symptoms for me several times when I couldn’t seem to kick a ongoing flare. It is not a diet I can keep up with tho, and I don’t believe its a “cure” but it did help temporarily.I went on Enbrel, and it helped tons (except for the massive hip flare I had this fall that came out of nowhere), so didn’t pursue the diet idea further.. I am far more interested in the research concerning gut microbes etc. I guess that’s diet related in a way. I spent a couple hours in the middle of the night last night thinking about this. The reason was my Significant Other woke up in the middle of the night with red swollen finger, with pain, came on in the evening, and went away during the following day. This is exactly how my RD presented with me, 2 swollen fingers (sausage digit, there is a fancy word for it, i forgot what it is) two months apart, different side, but same finger. After the initial swelling finger, my RD moved into other joints and I never had a fully swollen finger again. Weird
Last night he joked with me that I “gave him my RA” before he fell back asleep. Of course I laid awake thinking about this, I was a little freaked out about that statement. What if its something with the gut biomass, something that people have varying degrees of susceptibility to depending on their genetics, something that families share in both environment and genetics. After all, they discovered that ulcers were caused by a gut bacteria, and there is all sorts of other health conditions that they are now connecting to gut bacteria, or lack there-of…. this all kept me awake last night. In my next life I would love to be a medical researcher, ha! Meanwhile I just eat a lot of yogurt…
I hope he’s ok MJ. The microbiome question is fascinating, but could also be fraught with the same issues as DNA-mapping raised like individual differences in outcomes.
I think this is the word you were thinking of dactylitis. Hopefully I’ll have time to post about what my thumb did last week – the joint swelled so large that eventually the whole thing was swollen by the time I got to the doctor, which made him wonder if it was just a bad sprain – a bad thumb sprain – from what? 😛
dairy builds inflammation (needles in joints for me quickly)
Dairy is a huge part of the mediterranean diet
I do not think they took that into consideration very well.
There is no scientific evidence that diet influences RA. However, an overall nutritious diet containing the right amount of nutrients but not an excess of calories, calcium and protein is necessary. Regular exercise is important to reduce the risk of RA. Research suggests that eating a typical Mediterranean-style diet consisting of plenty of fruits, vegetables, and healthy unsaturated fats may help reduce inflammation and improve the symptoms of rheumatoid arthritis. Smoking and alcoholic beverages must be avoided at all costs as they are said to be causes of RA.
I have to comment – making changes in diet and exercise have completely turned around my RA this year. I even ran (yes, ran!) a half marathon this September. Just six months before that, I was failing (!) my fourth biologic and coming to terms with refractory (I don’t like these terms either) RA.
In March of this year, I did a 21-day fast with some friends for Lent. Completely for spiritual and not health reasons, we all spent three weeks without sugar, salt, animal products (meat, dairy and eggs), gluten, caffeine and alcohol. Within a week, my pain lessened. The never-ending joint stiffness started to let go. With lots of support from family and friends, I started walking for exercise. After we broke the fast, I continued to avoid dairy and gluten (I’m vegetarian but do eat eggs). Whenever I “cheated” on these, I seemed to flare and go back to the old way of symptoms. Before RA, I was a runner and with much support, started to jog a little, very slowly… only after walking for 20 minutes. Then one day, I ran a mile. I never thought I would be able to exercise again, let alone run, but exercise really seemed to help me. I have to go at my own very slow pace, but it’s exercise. And the more I go, the better I feel. Crazy. If I go more than a couple of days without exercise, I really notice.
I meet all the “poor prognosis” criteria for RA – high titre CCP-antibodies, high disease activity for over three years despite trying four biologics and several other drugs, age 37 at diagnosis (now 40). I’d gotten to the point where walking from desk to copier was a huge feat, standing in the kitchen was near impossible, and I needed two hands to brush my teeth or unplug my toaster. I was like this for three years – couldn’t reach anything higher than shoulder height due to shoulder problems. The difference is unbelievable. I have made dinner for my family every night this week AND even went to the grocery store one of the days.
“Best practice” is the buzzword of the day. I am an occupational therapist and work in research and am very well aware of the need for well-controlled studies, and they just aren’t out there to back up what I have experienced. But, good research starts with pilot studies, literature review, and feasibility studies for evidence to support a trial. Sharing even case reports is important, and I want to share this with everyone I talk to!! I keep challenging my diet and exercise program (since I can’t let anything alone) and it seems like an on/off switch.
I’m not sure whether it’s dairy, gluten, exercise, positive mindset and placebo effect :), answer to many prayers (YES!) or all of the above. I think it’s the last one (thank you, God!). I don’t know how long I will be able to keep this level of function (I do still have some pretty bad flares, had one last week where I could hardly get into bed or turn over with hip and knee pain), but exercised yesterday for an hour and feel better. Not all better, but better! Definitely more good days than bad.
I am thankful for every day. I am THANKFUL for the support of all my fellow RA-ers. I wish the best for everyone in our search for less-pain and more-function in our days… and the grace and peace to live in a thankful way for where we are, today. Peace! Mary
With a sed rate of 65 and crp of more than 6.80, I needed help fast. I could not walk down my stairs or brush my hair. I stopped eating dairy, grains and excess sugar and it strted to help but so SLOWLY, I mean mollasess slow. However when I tried Remicade and had a terrible allergic reaction during the infusion I was not too excited about trying a new drug, I was taking low dose prednisone for pain. So I stuck with eating raw fruts and vegs 80% and other stuff like a frappachino fr the other 20%. SLOWLY my labs went down 50 points every 6months. My knees took two years to get normal again. I am still at 6mgs of prednisone but I was at 15mgs. I still feel pain, but it was at 8-9 all the time, now its not. I feel in control, and I know my body is healing. My sed rate is now 19, but it took two years, and no ra meds except the prednisone that I have tapered down and down. I do not know what casues RA, but I know our bodies were made by a beautiful creator and can heal if we stop supressing it with harmful imm suppress meds…. My labs and knees prove it works.
My first major flare occurred when I was 31 years old but I was not diagnosed. We had 3yo and 1yo sons and I had weaned my youngest son from breast feeding. I had not smoked in several years though I was a social smoker from 18 through about 26 and I was raised around second hand smoke. I drank in moderate quantities during the same period.
From age 26 through 31, I had a very healthy diet with fresh fruit and vegetables and home-cooked healthy meals with limited meat probably three to four meals per week. My sons did not have sweets until their first birthdays. I had just finished losing the baby weight and weighed a healthy 125 at 5’5 and exercised regularly including long walks with my sons in their double stroller, yoga videos, and floor exercises.
However, I did experience a lot of stress during that period with my husband who was finishing grad school and starting his first professional job and also my work. The company I worked for was in the process of failing and being sold.
Overall, I would say I have had a pretty healthy lifestyle.
Since the flare that finally got me diagnosed, I have had more challenges since grocery shopping and cooking have been more of a challenge, but I would say my diet has been healthier than the typical “western” diet.
I have also been conscientious with supplements – taking a good multivitamin, D3, calcium, magnesium, and krill oil. I have also experimented with turmeric and ginger.
I am sero-positive for anti-CCP, RF, and other labs. My RF was 242 at initial diagnosis with GP and then 236 a month later with rheumatologist – if that matters. I don’t know how others test for RF, etc. other than what the lab reports show.
It all seems like blame the victim to me. So many people have offered cures for me – as they have for many of you. Mediterranean, gluten free, no dairy, vegan, juicing, and on and on. Of course, a healthy diet is important for anyone. And there are different genetic and environmental factors that affect individuals with RA. Not everyone is the same.
We won’t be able to pinpoint causes until we have genetic testing and then we can develop targeted treatment. Duh, people can be so IRRITATING when it comes to this stuff. It gets so old.
I have been vegan since April. Overall I feel that I am doing dramatically better. I am taking less medication that I did before and I am recovering from injury much faster so that there is no joint erosion. I firmly believe that there is a link between diet and RA.
I’m a little late to this party but found the article very interesting. I have been married 38 years and have three adult children. From the time my kids were young I have always tried to prepare healthy meals. I took red meat out of our family meals and substituted ground turkey for ground beef when my children were young. I always cooked fresh vegetables; I could count on my hand the number of times I have used canned.
In my family my sister and oldest daughter have also been diagnosed with RA. My younger daughter, as well as my father and brother probably have it but have not been diagnosed. My great grandmother as well an some of my fathers aunts also had terrible problems with arthritis but at that time were not diagnosed with RA. My great-grandmother had a hip replacement in the 50’s or 60’s. I truly believe that there is more of a hereditary factor to this disease that want we eat. I continue to eat well as I feel whatever we can to do naturally to help the better off we are.
i agree totally with Mary….ive had RA chronic for 15 years…the only thing that has quietened it down hugely….and helped me reduce my drugs….is the Paleo diet….the main culprits to aggravate an auto immune disease is Lectins which are present in all grains….all legumes… Dairy is inflamatory and causes …with the lectins…the degradation of the stomach lining…causing a leaky gut. The leaky gut is the main cause of all auto immune diseases. The Paleo diet is sugar, dairy, grain, legume free…..and it takes about 6mths -1 year to start to heal the lining of the gut……after this, you will see considerable postive change in your RA symptoms….and it works for all auto immune diseases. Diet is hugely integral to the healing of a disease…..and the cause of it.
I know for me that I am doing much better eating a gluten-free, dairy-free diet. I do even better when I can keep the sugar away too. I don’t know if the diet helps my RA, but it definitely makes me feel better inside and out – my guts just feel better and I have more energy. We have been going through an extremely stressful period, selling our house, buying a new house, moving, end of school year, busy at work, and I have faltered with the diet (sugar!). And yet, I haven’t had any joint pain in all this time (basically 4 months of continuous stress). I’ll repost if it turns out this is just the calm before the storm! 🙂
I was diagnosed two years ago with sero-negative RA and Secondary SS after 14 years of constant muscle and joint pain with chronic daily migraine. Hypothyroidism and Raynaud’s were diagnosed years ago. I am always happy to hear that someone has been helped by supplements A, B and C, or Diet 1, 2 or 3, alternative treatment like reiki, or religious faith. I have tried multiple supplements over long terms, particularly when it was believed I had a mitochondrial disorder, and I still take those with the best proven track records for migraines and RA. I’ve done the total elimination diet. I used to find relief with deep tissue massage and would love to get gentler massages, but massage…just not affordable at the moment. The worst I have ever felt in those 14 years was during the first two years, when I was exercising three times a week and walking daily. I am afraid that for me, praying did nothing…I consider myself spiritual, but non-religious. I think for me, speaking only for my own journey, attempting to reconcile that “bad things happen to good people” just made me unendingly angry, and agnosticism has helped me with that anger.
I absolutely do not discount anyone’s experiences with any of the above. But MY experience is unique, we are all special little PRD snowflakes. I take some seriously poisonous drugs that I would never encourage someone to take unless they were, like me, looking at life as far more of a burden than a blessing. I have been on narcotics for most of the last 16 years, I’m on MTX, Humira and low-dose prednisone, along with a number of other drugs mostly as needed. I am very fortunately someone who can take drugs like Ambien and Adderal and narcotics literally as necessary and stop taking them when they are not. They have made the most painful periods of my life livable. For those who can survive the 9+ pain sans narcotics, that is totally awesome, I salute you. I can’t, and honestly wouldn’t try at this point. It’s enough that I know my med use is directly correlated to my pain levels, my pain management doctor trusts me, and I experience some relief.
This site is wonderful because it encourages personal responsibility. Whatever a person’s experience with diet, drugs, supplements or religion, it remains our personal journey and responsibility to take control of our disease. After all those miserable, soul-destroying years of chronic pain and migraines without diagnosis, I own my choices. I once heard someone say they would shoot shark pee up their nose (mistake for shark cartilage supplements!) if they thought it would help their pain. So would I. I believe my magnesium, B-vitamin, Vitamin-D, SAM-E, turmeric and Omega 3 regimen helps…but not like the MTX, prednisone and Humira. What has never helped whatsoever is someone telling me that what helped them will absolutely work for me. Been there, done that, bought the T-shirt. Glad it helped you, but please do not think your experience should be in any way universal. Because I am a VERY special PRD snowflake! Right there in the blizzard of PRD with everyone else, just trying to find what will work best for me.
On that note, I have no disease correlation with diet, but totally believe a less-processed diet with less fat, high in fruits and veggies, will help out my methylation cycle and thus my energy long-term. I am terrible about veggies these days. So my next big thing is gonna be green smoothies. Who knows? It has to be better than shark pee up the nose! Though I’m not sure I will enjoy them more than my MTX injections, which are quick and painless. Green veggies….ugh…
My experiences and outlook echo yours. I am anti-CCP positive, with a positive RA factor. I was already vegetarian when diagnosed, so it wasn’t a huge step to wholeheartedly start a strict elimination diet with the absolute belief that I was going to figure out that I was gluten-intolerant or something similar and cure myself. It didn’t happen. My symptoms did not change at all, and neither did they when I gradually introduced foods one at a time back into my diet, over a several-month period. I’m all-out, whole-foods plant-based now because I feel better overall, but I have not healed myself and nor has God done so. I was a vigorous person before 2010, but now I exercise when I can, in moderation, or I risk send myself into a downward spiral for a day or a week or a month. I wish it were different: I’m glad for others that such efforts have been immensely helpful but I wanted to affirm your own experience. We have to be cognizant that what works for one will not work for all, don’t we?
Of course, I meant “RF” factor and not “RA” factor! This disease sometimes messes with my concentration, too.
Has any try Antibiotics ( Minocycline )
I was diagnosed with RA in remission about 3 years ago and it was only found by accident when i had a sore foot and an xray was ordered which showed erosions on my bones.
Since then i have done my best to manage it with supplements and now am trying diet restrictions does anyone have any tips.Id love to hear them.
I desperately do not want to be on medication so would love help. I believe 8 months spent on antibiotics due to tonsil problems was what triggered my RA as my immune system was shot as a combination of drugs and disease.
I have been diagnosed with severe RA for 20 years (I’m 35 years old), and I did notice a relatively major improvement when I became vegan (no animal products of any kind). Just this past year, I tried the Gerson Therapy for 6 months (a more strict vegan diet) with no improvement whatsoever (there are other factors to consider here, but it’s too in-depth to explain here). Out of the Gerson Therapy, I discovered coffee enemas, which have help alleviate the pain A LOT (don’t dismiss it until you try it. I give myself a coffee enema once per day before going to sleep). I have also continued juicing everyday. No real improvement yet, but since this disease was a long time in the making, I assume that it will take some time to go away.
I absolutely believe that what we eat is a major component to the disease, but even more than food, I believe that a lot of people with RA have very sensitive dispositions. I hear this from a lot of people––we worry about people’s feelings often and want to make everyone around us happy (generally speaking, of course). This can lead to a lot of internal “suffering”.
I hear that meditation is extremely helpful. For me, going on vacation is hugely helpful! I spent two days away from home at a B&B nearby with my husband, and I came back a different person. It was like I didn’t have arthritis anymore! Of course, the pain relief didn’t last once life got back to normal after a few days, but for a brief moment, I was blissfully pain free (well, just about, anyway).
So yes, I believe diet is hugely important (what could be more important than what we put in our bodies?), but I also think that it’s not enough to JUST focus on diet.
I have wondered about any connection very often. I watch my diet moderately closely and maintain a good weight for my height. I am mostly vegetarian, but eat dairy and some fish. I used to drink 1 to 2 cans of diet soda daily, getting my kick of caffeine to get through the work day. I yo-yo dieted from teens through my 30’s and avoided fat except some salad dressings and cheese. I often wonder if I became vulnerable to my RD because of missing nutrients that are fat soluble. I was diagnosed with hypo thyroid after my first pregnancy at 25 and my RD at 46 and in a stressful job (long hours/great people). I am now 60 and do OK – have had to modify lifestyle greatly (early retirement, restricted gardening abilities, night driving-thus not going to evening activities that I would be too tired to attend anyway). I quit the soda, watch, but eat the fats, and have maintained my bones at a moderately unhealthy level, but not declining any more in the last few years. (used to be on Fosamax, but it made me dizzy and I couldn’t walk which is therapy too) No family history of RD, but there is on hypothyroid-I am the worst and the youngest diagnosed. I live in the north and from a big family. No medical providers have ever asked what I eat, but it seems so key to treating many things, but more importantly – prevention before the vulnerabilities set in…
YES it can help. I have tried Humira, remicade, mtx, prdenisone, cortisone, sulfasalizine . Remicade nearly killed me and gave me a heart attack, my blood pressure was 120/80 when I got to the infusion room then it went to 250/118 in ten minutes. SOOO, I tried a eating raww OH MY GOSH the pain was so much better, it was still there ,,trust me but it felt so much better. I have RA pain in my sternum, wrist, knees(drained 20 times) ankles,twisted toes. Juicng veggies such as cucumber celery and carrot once or twice a day and avoiding grains , suagr and dairy had made a bigger difference tgan all the meds I tried. Last thing, some meds casued me to flare such as mtx, I felt so much worse on that stuff, it was like the days I cheated and ate cookies, same reaction, big swollen knees that dont bend, that stuff kills cells.
ok i already have RA , what type of diet should i be doing, i get so confused from keto, to paleo to high protein , i have discovered there is to much bull sh;t on the internet , does the anti inflammatory diet work , i believe if God created it then it cant be bad, someone please tell me what to do. i am so tired, i have been searching for a long time. , one place stevia is bad, another its good , one place low gluten, I am so confused, i just need plain and simple please