Rheumatoid Arthritis Swelling, Take Two
Rheumatoid Arthritis Swelling (UPDATED 2016)
In honor of the blog’s 2nd birthday, let’s consider some issues that have been significant over the last two years. Today we’ll consider Rheumatoid Arthritis swelling. This may be blunt. More like a frying pan than a sword.
Talking turkey on Rheumatoid Arthritis swelling
A couple of years ago my kind-but-clueless-what-to-do-next (her word) rheumatologist told me two things that provoked my online journey to go deeper and farther. After two and a half years on high doses of Humira and methotrexate, my RA symptoms were not improved. Disability progressed even though obvious external swelling had mostly subsided.
Two significant things Dr. KBC (kind-but-clueless – her word) said:
1) I don’t have a clue what to do with your RA. It does not look typical any more.
2) You cannot have x-rays done because you have a systemic disease. There’s no justification for x-rays.
I searched online for patients like me. I searched for some kind of explanation why my RA hurt more than ever, with constant fevers, and joint instability. Why did some claim those symptoms are only possible or relevant if obvious external swelling is present?
I listened to patients and blogged for almost a year before I made my Rheumatoid Arthritis swelling confession. But, there are 224 331 358 370 replies on that post. If you’re confused about Rheumatoid Arthritis swelling, you could learn a lot there.
When I got the courage to leave Dr. KBC, I met a series of rheumatologists who either insisted that I was in remission or that I really have fibromyalgia because my “inflammatory indicator” CRP and my swelling both say I’m fine. Each of them was adamant.
Like Goldilocks, I held out for the one that seemed just right. Did you see me cry in the Good doctors treat patients video? We were overjoyed to finally meet Dr. Smart Rheum who said wonderful things like this:
- “You DO have swelling. I can feel it when I examine your joints.” (Examining my joints was a novel experience.)
- “Tests don’t always show disease activity. You have to look at the patient. It’s the patient that matters.”
- “What do they mean ‘You don’t look like you have RA? What does RA look like?’”
- “Swelling does not have to be on the top of your hands. The other side is swollen.” (Where the tendons are.)
Last week Dr. Perv told me “You have no kind of arthritis at all. You have no swelling. You claim to have pictures of swelling, but you have none.” I said, “My knees are swollen right now-” “NO they are not!” he interrupted without ever looking at my knees.
Note well: most “asymptomatic” patients have synovitis & bone edema
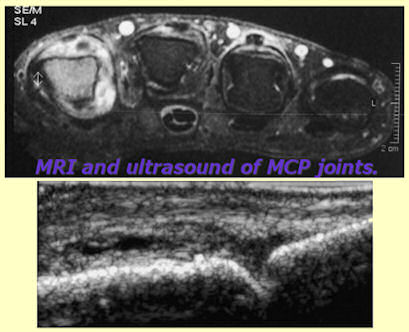
There are some links to support our case on that first swelling post, but there’s one I somehow missed until recently. Dr. Brown’s study at the American College of Rheumatology (ACR) in 2006 showed that patients who rheumatologists label as “in clinical remission” due to lack of visible symptoms are experiencing damaging disease activity. Active synovitis and internal swelling can be detected with skillful use of the appropriate tools. Bone marrow edema is another critical unseen aspect that doesn’t look like RA to the naked eye.
“Even in asymptomatic patients with clinically normal joints, MRI showed that 96% had synovitis and 46% had bone marrow edema, and ultrasound imaging showed that 73% had gray-scale synovial hypertrophy and 43% had increased power Doppler signal,” they report. Mild synovial thickening was seen in three of the 17 control subjects (18%), but none had bone marrow edema. Brown et al point out that synovitis in RA is a link between inflammation and structural damage and they predict that the patients in this cohort who had synovitis are at risk for subsequent structural damage. They suggest that such persistent, active synovial inflammation may explain the adverse RA outcomes seen even in patients who meet the ACR and DAS28 criteria for complete remission. This is a large study and needs to be taken seriously,’ said Professor John R. Kirwan, consultant rheumatologist and professor of rheumatic diseases at the Bristol Royal Infirmary, in the UK,” RA Remission Often Accompanied by Silent Synovitis.
Was it? Taken seriously? Maybe more rheumatologists need to hear about it.
Now I finally have persistent swelling. My knees have had Baker’s cysts behind them for almost a year. They’ve been painful and stiff for five years, but now I have something that brings a little sympathy. The fronts of the knees also swell periodically.
“Asymptomatic” is in the eye of the beholder.
Now I have an opposite problem. They deny that THIS is swollen.
Read my lips. I’m. Thin. These are not fat knees. They are swollen.
I went through the same thing with my pregnancy with Roo. My feet were can’t-wear-shoes-huge, but the midwife said they weren’t swollen. After Roo was born she remarked, “Oh my god you’re right – your feet are skinny.”
Enough.
We don’t have time for it. We are supposed to be treated “early and aggressively.”
How can we be if so many doctors don’t recognize RA because they have a wrong mental picture of it?
So why does this myth persist?
Happily, others are speaking up about Rheumatoid Arthritis swelling also.
Edit: Link to original Musculoskeletal Report article updated to a current link to the Brown swelling study, here:
ARTHRITIS & RHEUMATISM
Vol. 54, No. 12, December 2006, pp 3761–3773
DOI 10.1002/art.22190





Hi Kelly, I want to pick up on 3 points. Firstly X-rays. I’m in the UK & when I was dxn 20 yrs back I initially had hand and feet baseline x-rays, so they had something to compare against as time went by. Before starting mtx 18 mths or so later (first dmard didn’t work plus I was pregnant at the time),I had a chest x-ray, again baseline. I now have secondary OA in the hips & have yearly x-rays to see how the degeneration is going, thankfully its slow.
I also wanted to say that more recently I’ve also been concentrating on my main pain area in any given apt, mine are 6 monthly at the moment. I always give him a brief run down of what’s hurting (he always asks how I’m going and what my pain has been like), & I make sure he knows all the areas I’m having pain in, but I make a point of saying ‘But my main issue recently is….’ I have found this leads to a focus on that joint/s (shoulders being my primary issue of late). This has led to a full exam of that area, although he always checks my hands, knees, hips and upper range of motion and we’ve discovered 2 visits back that I have the start of secondary OA also.
Lastly (sorry this is long), I have found with this rheumy that being proactive & letting them know you are knowledgable about your disease helps. I feel that my rheumy has more respect for me as a patient who is an advocate of my own health, and that I’m not going to be blindly led by what ‘any’ health provider says without my own research and follow up. I’m polite and I always listen to his advice and ideas but likewise he pays me the same respect and courtesy.
I wish for you that you will find someone as wonderful who will treat you and your RAD the same way.
I have had a knee replacement, but my knee is still swollen. I have had surgery on my wrist, but my wrist is still swollen and becoming lumpier by the month. Both my wrists have lumps and are painful. My other knee is not swollen, but is painful. I still have not received an absolute diagnosis of Rheumatoid Arthritis. My Rheumatologist calls it “inflammatory arthritis”. This makes it very difficult to convince my supervisor that I’m really ill when I miss work. I don’t understand why it is so difficult to get an honest, real, true, diagnosis. Are the doctors afraid of something? Possibly the insurance companies? I just don’t get it. Maybe this is why they won’t recognize these issues.
Please HELP! My symptoms start almost two years ago now and I have no diagnosis yet but extreme pain in my fingers. Many other joints hurt as well but my finger are cripplingly (not sure if that’s a word:) painful and interfer with my daily life. I cry myself to sleep many nights because the pain is so awful when I do move them but even worse when I just lay them on my pillow. Morning they are very stiff and thick but not as painful. I do not have visible swelling and all of my blood work is 100% normal. I am on my third rheumy and he seems promising but at the same time says he does not believe it is RA because of the lack of swelling and lack of inflammation seen in blood work. He says he believes that my symptoms are “real” but does not understand why the pain is there when there is no swelling. He says that he will do his research but I would really like to be able to just hand him a stack of research when I see him again in 4 weeks. Any advice???
Thank you for this website and your honesty!
April
This is the problem I’ve had too. I have had swelling but my rheumatologist has never seen it. I’ve had other specialists who have seen it, diagnosed me with synovitis and have felt my hot/swollen/red joints, but my rheumatologist just doesn’t believe me without seeing them for herself. I’ve had a bone scan which reviled some inflammation which my rheumatologist initially thought was enough evidence to say I “definitely have something going on”. Now she’s taken that all back and says it’s nothing. My blood tests show nothing too.
Anyway, my rheumatologist has put me on Plaquenil. They were prepared to put me on a 6 month trial. It is a DMARD but not as potentially harmful as Methotrexate. It’s used for mild RA, Lupus and Sjogren’s. I’ve been on it almost 6 months and it’s dramatic. My morning stiffness is minimal, no swelling, still a bit of pain, but there’s a huge improvement in my joints and fatigue. I’ve even had improvement in my nose/mouth ulcers. Do your own research, but you could ask your rheumatologist if he/she would be prepared to trial you on Plaquenil.
Good luck.
My joints do not swell as a rule. I have had some swelling, with pain,but it does not look like the pictures. I had to smile about the remark about the top of hands weren’t swollen, the other side was. Mine often are. The bottoms of my feet swell and are quite sore. Interestingly enough, I have not had abnormal CRP results at all. My doc says that I have RA anyway, based on the minimal swelling and 600 RF factor. He is treating aggressively. But if swelling is used as proof of RA, I probably would not have it!
Unfortunately I’ve met a few drs who do decide entirely by that. Whether it is present or active. I believe it will be the way of the past, but not yet unfortunately, according to some sad letters I read.
But, I also thank you for posting about how your good dr treats you – that gives other people hope they will find help too.
I cannot believe this, this is a first for me! My feet hurt terribly and my right knee with the Bakers Cyst. Until I read that you, Kelly were dealing with the pain of a Bakers Cyst, I was made to believe it had no bearing on the fact I suffer with RA!
I was told nothing of the sort, only, ” It’s only a fluid build up behind the knee.” I am in so much pain, and all I am given are extra strength tylenol.
It does hurt yes. And RA can exhibit as bursitis, tendonitis or other forms of inflammation and lead to Bakers cysts or carpel tunnel or many other things. I do know what you mean though – since I’ve heard it from a thousand people and had it happen to me. Sometimes a dr doesn’t understand what it’s like to live with that symptom and just dismisses how it affects you. You can try to explain how much having these on your knees can limit you and ask what can be done about it. Tell the dr that the tylenol is not an does not reduce inflammation or swelling and does not give you any relief from this level of pain. And mention what you can’t do – for example, I have them on my knees too and I can’t sit with my knees hanging like on a barstool. And sometimes they do not straighten after sitting.
I hope he listens.
You mentioned that your fingers got bigger kelly, earlier, is it possible for this to happen to the tops of your feet/toes. i’ve been at 8 1/2-9 my entire life, none of my 9 shoes that go over the top of my foot (like, crocs, anything that isn’t a flip flop) fit now. I’m in a solid 9.5. I keep wanting to ask, if this normal? That and I feel like both wrist joints are poking out/swollen today, like I need some kind of pictorial to show people i’m not crazy that this is happening to my wrists and feet.
Meerkat, since the beginning of this year I have gone from a D width being loose to a 2E feeling about right and sometimes that is tight. My feet are a mess but they aren’t puffy at all.
Hi, I see a new Rheum. doc. tomorrow. I’m praying that this one will be a Dr. Smart Rheum. like yours.
Thsnk you for this!
Wow! What a breathe of fresh air! It is amazing that there is someone who gets it! Actually many people! I’m am not alone thank you! My family doc and Rheumy have focused so much on my CRP test more than anything else and I have had no idea why it’s been low! Maybe my body process inflammation differently? it seems to do everything else differently! I do know how much I suffer with the pain in my tendons and joints. I get inflammation in my left eye only that lasts for usually only a couple of days. My hands, wrists, neck, shoulders, back and knees all take their turns too in causing me to suffer. I am positive for RA factor which recently increased levels and my thyroid is out. My Rheumy is away for the next week so we will see what he says about results now?
Thank you so much for your blog!
Hello, i feel that i noticed you visited my web site so i got here to return the favor?
.I am trying to to find issues to improve my web site!
I suppose its adequate to use some of your ideas!
!
Kelly,
Like you my hands and feet are skinny so swelling is not always noted. My first Rheumi was wonderful. She would gently palpate my hands wrists, feet and ankles. Beside being a kind compassionate person, she also had RA and understood the subtleties of the disease. The problem with most doctors is that they Do Not Listen!!!!! to the patient.
Since my first doc moved to California, I have not found another here in Fla.
I am confused about the swelling issue as well. Every time I’ve been to see the Rheum they casually look at my hands and tell me they don’t see any swelling. I had a MRI of my right hand last summer because my hand curls up and I have pain in the wrists and fingers (both sides but worse on right). The MRI revealed “Two punctate nodular foci, markedly T1 hypointense and T2 hyperintense, with associated interval enhancement within the region of the mid lateral aspect of the hamate bone measuring less than 5 mm. Also at the subcortical region of the later aspect of the distal epiphseal region of the 3rd metacarpal…no definite increased synovial thickening, hyperintense signal or enhancement in the carpus region ‘otherwise’. Also noted, “Partial tear of the distal-most aspect of the flexor pollicis longus tendon, with moderate to marked tendinopathy/tendinosis.”
I like how the report states “otherwise”. From what I’ve read about MRI imaging of early RA, the T1 and T2 results that I have are considered synovitis. Other googling about why I would have a partial tear of this tendon also took me to several articles on RA.
I know I’m no MD but I am a RN and have some understanding of medical literature. Why is the report saying no “definite” swelling and using the term “otherwise”? I can barely use my right hand at times and it curls up and I can see exactly wear this tendon is torn as I have a large lump in that location that can be clearly seen.
I was sent to a hand surgeon who picked up hand and moved it around a little and stated that he didn’t think I had a torn tendon. ??????? So who is right, the radiologist who read the MRI or the guy who looked at my hand and said “It’s probably tennis elbow.”?
I don’t get it. I am loosing the function in my hands and just typing this little bit is hard for me to do.
It is so frustrating. When you can feel the constant pain in your wrists and ankles and you can see some sort of weird white nodules and white lines on your fingers and toes that were not there before this pain started, and you can see lumps forming on your wrists, etc. and no one seems to know anything and you wonder if they really believe you. But after 3 years they finally did start me on Methotrexate. I just started my 3rd month of 10 mg weekly and there are days where it’s a little better and I wonder if it’s starting to work but then here I am again today with pain all over especially my wrists and I wonder. It’s so hard to live like this and I keep praying that relief will come. The thought of being like this the rest of my life is a constant dagger in my heart. I need to try to stay positive and do the best I can but it’s a daily battle. Sorry this is a bit long winded but the topic of swelling is confusing to me. Anyone know anything else about MRI interpretation? And what does it mean if the Dr. seems to blow it off?
As a retired RN,I have seen doctors blow off patients and their families because they haven’t a clue. My last rheumatologist asked me(on my first and last visit) “now what would like me to do for you?” Excuse me!!!!! My answer, “Not a damn thing.”
Well, off on the great hunt. Everybody take care and fight like a girl
w
I had sort of an atypical presentation, I suppose, with massive swelling and deformities of both ankles and feet(but no pain). I thought it was related to a recent dx of Hashimoto’s and pretty much blew it off. Fortunately, I took photo’s of the swelling (9.8 lbs of it that literally happened overnight). We were joking about it at work. I had no shoes that I could get into. My GP gave me Lasix, and I reluctantly took it (didn’t work).
Eventually it went away (about 2 weeks), only to reappear in my knees. This time there was crucifying pain with it. I couldn’t bend my knees. I couldn’t get off the toilet. I had major trouble getting up the stairs at home, and I was struggling to finish my 13 hour night shifts. At first I thought it was related to a new work out that I was trying, and just did ice, Ibuprofen and Tylenol. I am an icu RN, so I probably should have known better.
I thought in the beginning it was a torn meniscus, but when the other knee started up a week later, I knew something was up. Fortunately, I took photos of this as well. When I saw my GP, I was lucky to get a course of pretty high dose steroids while waiting for my Rheumatology appointment. Felt great within 2 days. Of course, all my inflammatory markers were normal at Rheumatology, likely from the steroids (which I can’t seem to get off of now).
Now I have pain and mild swelling in my hands, feet, ankles and knees. I am fortunate to have a caring Rheumatologist who did start treatment right away.
Looking back…there were episodes of swelling in both thumbs. I blew this off to the heavy bag I was carrying to and from work. For some reason my entire left side is always worse. No idea why. I do not get redness with the swelling very often. But I had terrible pain with the thumb swelling. I thought it was an injury and was tying ice bags to both hands at work in between seeing patients. I couldn’t open medications at work (much like peeling stickers…removing lids…etc).
Never once during all of this did it occur to me that this could be RA…until my knees swelled up.
I need some advice………they can’t make up their minds up about what i have!!! I don’t fit the bill….blah blah!! Bloodwork seems good but just because I have swelling of my knee I automatically have RA! Methotrexate scares the hell out of me…….and all of the other medications too!
hi Tammy. It can take a while to be sure – you may need a second opinion. Early treatment is supposed to help a lot so it’s frustrating to not know. There is some info here that may help with that: https://www.rawarrior.com/do-i-have-rheumatoid-arthritis/
You guys if you rheumy doesnot work for you find another, we are paying them, even if it is our insurance. I would not fire the old one but i would get your insurance book and find the list. That goes with all docs. When i started with ra my kneess where the only thing that was swollen i went to 3 different orthro docs before the last one realised that there was something different than oa, he sent me for some bloodwork and made me an appointment with my ra doc. My ra doc does listen to me and always sends me a copy of my bloodwork. I was having a lot of swelling in my feet and legs with my current drug regimine i took pic with my smart phone and showed him we added xtra meds. They have to,work for you or they are no good. Not all of them are bad.
My experience is different, too in that I have no redness or heat (possibly the raynauds’syndrome offsets it) in my hands/wrists/shoulders/knees etc. I usually do have swelling, stiffness and PAIN or aching in my hands and wrists. Since I have several other autoimmune diseases my rheumy put me on methotrexate and prednisone. He felt that clinically I have RA even if seronegative since CRP and some other markers were fairly high. I think what’s really helping the most is LARGE doses of high omega 3 fish oil daily for the last 3 months to combat inflammation. Has anyone else tried this, and how did it work for you? My fingers and wrists are still swollen and stiff, but the pain is nearly gone (for now…)Grip strength still lousy but oh, well! I’m pretty new to this so was glad to find this site! Thanks
I was diagnosed 7 yrs ago. I live in constant pain in my neck, hands, knees, ankles, feet, hips, wrists, shoulders…… I have swelling where ever I have pain! I have no insurance right now, so no treatment. None of the rheumy’s I’ve been to will prescribed pain meds, only NASIDS, MTX, & Biologics. I was going to a pain mgt Dr to get pain meds. I can’t afford either right now w w/out insurance. I’ve had this flare going for 8 weeks. I am at a loss here. My family is sick of my being sick & to tell the truth so am I. They are sick of having to help me all the time. My house looks like an episode of “Hoarder’s”. I’m just so sick of it all!!!!! I don’t know what to do. No one here has any sympathy/empathy left. They say when I say “I can’t do…… ” They say “Yea, we know. What CAN you do?”
Dunno who says that Theresa & I hope they are joking. The answer is you CAN always smile – well most of the time. The rest of the time, you CAN sympathize with so many of us in the same situation.
I hear you & I’m very sick of it too.
Oh no they aren’t. They want the mom & wife I used to be. I cry. I beg. I do nothing & it piles up to the rafters. My right hand (I’m right handed) is starting to curl & I can’t grip anything w/it. Hubby helps some & came home today so he could help me clean the mess the kids REFUSED to clean up for 3 days. I was so AWFUL to them when we got home from school today. My 16 yr old daughter said to me “Oh just HUSH! Your the mom it’s your job to clean up after us!!!!” I’m currently only speaking to my husband. I just want to cry most of the time. All I have is my faith in God. Thanks so much for an understanding shoulder.
Dear Theresa,
I’m praying it will get better. I’ve been through similar things at times & it’s awful to hear that. Of course this is not your fault & you’d much rather be able to do everything.
Thanks so much Kelly! I’m praying too, for you & me. Think I’m going to bed early. (I’m cold!)
Thank you, thank you, thank you!! I was diagnosed when I was 12 with RA. I was diagnosed at age 21 with fibro. Lately I have been experiencing more diffuse and odd symptoms. My rheum doc, who is new to me and is the only one in our system who is nearby, stated that he doesn’t think I have RA. ARE YOU KIDDING?! I have visible joint damage on x-ray, my fingers are turning outward, morning stiffness x4 hours, etc. But since I don’t have classic swelling and heat at the joint, it must not be RA, according to him. I have been on every NSAID (until gastric bypass 2 years ago) as well as gold, Humira, Enbrel, and most recently Remicade (to which I responded to ALL, although with varying degrees of success). He took me off the Remicade and methotrexate and I have been off all meds for nearly 4 months. I cannot take prednisone because I don’t respond well (in addition to not working it wreaks absolute havoc with my meds — not great when already bipolar). I have been in absolute pain for months. I am now driving 3 hours away to be seen at the University of Wisconsin. And I am betting a million dollars they say it’s RA and fibro. I honestly wept reading some of your posts because I have felt very alone, like I must be going crazy because I have these symptoms but again, it CAN’T be RA. I have known how to treat the RA for 26 years and have had to deal with symptoms and modifications that come with it. Now I am expected to believe that even though the only change has been worsening symptoms that it’s suddenly gone. I see the rheum at UW-Madison in 10 days and it can’t come soon enough. I can barely get out of bed let alone trying to care for my young family. Thank you so much for helping me to feel as if I am not completely insane!!!
This fits me to a T. My Rheumatologist sent me to a specialty RA clinic and they are now trying to tell me after 33 years of this dx that I don’t have I
RA. I don’t fit their guidelines and do not have swelling. They are swollen to me, stiff and painful. She is trying to label me a fibro. I refuse. She ran a bunch more tests and a bone scan so anxiously waiting to see what the tests all say. I was so upset after my appt with them I cried all day and cry every time I think about her words to me that day.
Hi everyone. I just found this website and after about an hour of the tears flowing from reading other’s stories, and getting that validation that I so desperately needed, I am so truly thankful. I went online looking for any information I could find on lack of visible swelling but still having active Rheumatoid and I found this website!! Thank you, thank you!
I will try to keep this short before answering the questions regarding this post. I am 48 year old female and have had RA since I was 29. My RA has been fairly aggressive and since 2000 I have been on social security disability and had to quit working as an RN. I actually use to work for my current rheumatologist as his office nurse/RN. Funny how things turn out in life. My right hand and wrist is almost completely unusable. I had a wrist replacement done about 5 years ago, right thumb fused due to severe subluxation and multiple tendons have been repaired due to rupture. I currently cannot grab anything unless it is large enough for my hand to fit around. Anything smaller than that and I could be an hour trying to pick up a pill that I dropped on the floor. My left wrist is heading in the same direction.
In regards to question 1)RA swelling? Do you have it all the time? Does a joint ever hurt and creak without much swelling? Has your pattern of swelling changed over time?
Yesterday my rheumy Dr “It Remains to be Seen” told me that due to visible lack of swelling in my joints, my RA MUST NOT be active. Even though I have had RA for nearly 20 years and I know my body way better than anyone else. I feel like I have the flu, sometimes I can barely make it out of bed to just even get to the couch, multiple joints are hurting. But I DO NOT have a fever, never have in fact since I was diagnosed. And he could not see or palpate any swelling. Yet my left wrist is extremely painful to move and has been slowly getting worse. He will not xray it because he says the pain I am feeling in that wrist is due to the previous damage and there is no need to re xray.
I came home so discouraged and started researching if it was possible to have active RA and current damage going on without visible swelling and I found this website. I actually found other sites that documented that this is possible. I also remember my hand surgeon telling me that even though he did not see any swelling on my right wrist before he operated on it he KNEW that there was current inflammation inside the joint. He did xray it and turned out I was actually missing some of the smaller bones in the joints space. They had simply been eroded away. So sad that my rheumy would not listen to me over the past few years and waited so long to send me somewhere to get it evaluated. Could have possible avoided me having to have a wrist replacement.
2)RA Inflammation markers
Have you ever had a normal CRP blood test result while you still had RA pain? Do you ever have normal ESR / sed rate result while you still have RA pain?
During my 19 years of RA, the one and only time that I had an elevated CRP and sed rate was early on in my disease and it was when I had completely been taken off of prednisone. That was it. Those labs have been totally normal since then. And I have pretty severe deformities in my hands, wrists and feet with multiple surgeries. I have RA pain every day, all day. As I am sure most of you do as well.
Doctor’s comments
Has your doctor ever told you anything similar to…? “I don’t understand why you say it hurts because I do not see swelling;” “Perhaps this pain is due to something else because your inflammation is under control;” or “Your joints look good. Your RA is under control. Maybe you need an antidepressant or….”
Well, that is why my rheumy is called Dr It Remains to be Seen. Because he ALWAYS sees that my RA looks great, I don’t see any swelling. Your joints look great. You should be so grateful compared to some of the little old ladies I treat. I feel like saying well crap, they are elderly patients who were not treated aggressively back in the day that they did not have access to the meds we do now. I am 48 for pete sake’s. I should not have this much damage at my age! Sorry, I am really cranky tonight.
So sorry this was such a long rant. I wanted to answer all 3 questions since they all currently something I am dealing with. I have been begging my rheumy to switch me back on Orencia IV because I do not feel that the Actemra IV is working effectively. But based on lack of swelling, forget it. He won’t even consider it. So, I am now searching for a second opinion and also looking for a hand and wrist surgeon that has experience with wrist replacements.
If anyone knows of a multi specialty clinic that I could research that has both Rheumatologists and Orthopedic Hand and Wrist surgeons that perform wrist arthroplasty, I would truly appreciate any info. At 48 years old, I do not want to give up on the use of both of my hands. I have too much of life I want to live and enjoy. My first grandchild will be born in August and with my current situation, I am not going to be able to help my precious daughter change a diaper or even pick up my granddaughter. I need help!! Anyone??
Thanks to all for taking the time to listen to rant and rave. Sometimes it just feels good and I know that the people reading this will know what I am going through.
I’m so glad I found this link! I was dx last year with RA after 5 or so years of random symptoms. I always tested slightly positive for RA and had slightly high inflammatory factors but not enough for any Rhuematologist to take my symptoms seriously until I found a really compassionate one last year. My current Rhuematologist has been great so far and started me on methotrexate and steroids last year and what a difference that made!! I had always had problems with painful joints but mostly in my hands, wrists, and knees. I was getting to the point that I hated to shake anyone’s hand or have to go up any stairs but even with all that pain, there wasn’t really any visible swelling. I started the meds last August and was feeling better than I had in a very long time!! UNTIL December when my doc decided that I needed to stop the steroids. He felt that since my labs were showing that all my inflammatory tests were coming back really low that the methotrexate should be able to handle the RA. He tapered me down for a month but little by little the painful joints started coming back. I told him at my appointment in Feb. but my labs were still good so he seemed to think it was just the weather aggravating my joints. (Because I live in the Chicago area and our winter was the coldest I ever remember!!). It is now August and my joints hurt on a daily basis since June. Sometimes I even hate to go to bed and lay down because my wrists and ankles will get a dull throb in them. Even with as painful as they are, I only have mild swelling. My ankles and feet hurt to walk most of the time and it’s really bad if I get up in the middle if the night and in the morning. The fatigue has been pretty bad too. I did tell my doc about it in June but my labs were all good so I didn’t have any active disease going on. This is so frustrating because if the RA isn’t active why do I feel so bad!! I have also had several flares of scleritis (which was one of the first symptoms of my RA). My doc has been really great so far but now I feel like he thinks I am overstating my symptoms. Reading all if the other posts has been great though so I don’t feel so completely crazy!!
Yes my Doc told me my RA was well controlled and that everything else I was feeling was the fybro. I am seronegative and still have pain and some swelling especially after or while I am doing something physical. I ice them and it helps, I was told by an RA’er that it was the damage that was already done that was causing my pain and swelling. My RA was basically diagnosed by the xray tech. Not the Rheumy. My swelling is mostly seen in my palm side not the other side but my Rheumy always turns my hands over and says there is no swelling. I am frustrated, I don’t know what to believe. I do have more energy but that is since I started the Lyrica. BTW my Rheumy has gotten my scrip for Lyrica to be written out by my GP now and a little note on my script says she wants to see me in her office. Don’t know what to do anymore alas my options are VERY limited as to Rheumys.
Have never had abnormal lab. Even when I couldn’t walk or use my hands. Was diagnosed by a Rheumatologist in 2004 after every test in the book to r/o everything else. Finally biopsies a “place” on my hand which was a Rheumatoid nodule. I am also thin. My hands were so bad, the weddings rings that were welded together came apart. Have been on meds since then and have never been that bad again. Thank God.
I can be in incredible pain with no visible swelling. Only rarely will swelling be obvious. And yes, the assumption is always that it can’t hurt if it isn’t swollen. So wrong! Some of my worst days are not accompanied by visibly swollen joints.
After a 4 year post illness from mis diagnosed hepatitis c ,I had ecoli septicemia which shut down my kidnwys and liver. On dialysis for a week. Had to eremind rhem to draw labs in morning following dialysis. The total hospitalizTion was a disaster. Acused me of alcoholism . Gave me wrong antibiotics for uti that caused the septicemia. Long story short they discharged me 2 weeks later,still with low grade fever,joint pain unbearable and fatique. I had to come to mexico to live as I was. Travel nurse and my housing and mex insurance were tied to my contra ts. My husbands family took us in. When the hospital discharged me they told me I needed a new liver and had months to live. So,I ztarted getting my affairs in order. I went to aee a hepatologist here. She found they had discharged me with an active urinary tract infection,fever ,high white count and intense joint pain. After 3 visits my liver enzymes began to normalize,kidney function normal and then she suggested I had RA and the infection overtook ne because of the immunological compromise.
She saved my life! I am seeing an incredibke rheumy. Unfortunately there are no narcotics in mexico so my pain is managed with tramadol. On plaquenil and methotrexate. Still have bad flares but we are working on it.
I would not be here if it aeren’t for astute Mexican drs. By the way I am a registered nurse with 32 years of icu experience. All those swollen joints and pain prior to my critical illness I attributed to my job and getting old.
Never ignore your symptoms, always get a second opinion and have a health care friend in case you are hospitakized designated to follow your care. I an thankful for every day I wake up with my pain and all.
I’m on my third rheum now. My orthopedic surgeon is the one who referred me after carpal tunnel surgery then I was in his office every couple weeks with a new joint affected. The first rheum did tons of blood work and after finding elevated ANA but nothing else to support it she offered to send me to the university hospital where they would likely put me on antidepressants and toss me into the fibromyalgia bucket. I said no I’m already taking them and it’s not helping my joint problem. She them asked me what I wanted to have. That was my second and last visit with her! The second guy was a quack and he wanted to throw meds at me but gave me absolutely no indication as to what he thought I had. After two visits with him and leaving his office in tears I was ready to give up on the medical community. My orthopedic surgeon didn’t give up on me though. He told me I’m too young for this (this all started when I was 35) and he told me don’t let anyone tell you that this is normal ageing! He pushed me to see another rheum. I saw the new, awesome doc about a month ago and he said that there is no doubt in his mind, I have seronegative RA. He did ultrasounds and X-rays right in his office. He started me on a prednisone taper and Plaquenil. The steroids worked so well and as soon as I started to taper I was back to square one. I go back to him in 2 weeks, 6 weeks since I started meds and he said if I’m not feeling much improved he will add MTX. He will give that a certain amount of time on the MTX and if my results aren’t good he will add in Enbrel. He said most patients feel better overnight on Enbrel but he had to follow protocol. He was so compassionate and so confident that he would get me feeling better. He just asked that I’m patient while we get the right combo of drugs that works for me. He has brought me much needed hope! Right now I’ve been getting terrible headaches that last for days and ibuprofen doesn’t work. Idk if it’s the RA or if it’s a side effect of the Plaquenil… Just before my RA diagnosis I was diagnosed with pernicious anemia and iron deficincy anemia. I’m self injecting B12 and that has helped some. The hematologist thinks that my fatigue will greatly improve once we get my iron levels up. I’m actually waiting for a call back today with results of blood work from last week. She may need to do weekly IV infusions to get my levels up. She says I’ve got a double whammy with the RA and low iron fatigue. my best advice if your RA doc isn’t helping is to seek out others until you find someone willing to listen and help you. My old PCP was trying to manage my anemias and I wasn’t thrilled with how she was going about it. I found a new PCP who said that my problem is complex and that a hematologist was the right doc to manage it! I’m telling you a great doc makes all the difference! It was almost 2 years after onset before I got the 3rd rheum doc and the diagnosis. The first rheum visit was 5 months after onset. I didn’t not have as many shmptoms or as many joints involved and my swelling is way worse now than it was, but I wonder if I had gone to doc # 3 first if I would have been diagnosed and started on meds and if I could have avoided the progression that I’ve experienced. I beg you all with doc’s your not happy with to please make appointments to see others and see who you like and who listens then you can switch if you find a better match!
I started Humaira. I’ve had 3 injections. Now I can’t move. Every joint in my body is swollen. My hands look like a claw. And my dr. wants me to stop pain meds? How is that posable. He said the norco will hurt my liver. wtf does he think the humaira and luflidamide is doing to my body? Anyone else have to go without pain meds. He wants me to go to a pain clinic? I CANT MOVE MY JOINTS, i don’t want yoga and !@#$%^&*()_. Thanks Robin
The move in the US to stop allowing pain meds for RA / RD is disturbing and destructive because it’s one of the most painful conditions known and does not have a cure or any way a person can prevent it.
The tylenol (acetaminophen) in the norco can hurt the liver at higher doses, but it should be safe taken as prescribed, depending on whether there are other liver risk factors.
I’m having these issues at the moment! Rheumy insisting that I also have fibromyalgia due to them not seeing the inflammation correctly! I too have bakers cysts that worsen the longer I’m on my feet. I can’t wear normal shoes/boots. My fingers and wrists are always swollen and I’ve now got swelling around my hip. I don’t work and couldn’t at the moment. In may they were gonna introduce biologics if no improvement it’s now Dec and they still haven’t!!!!!!!! I’d like my life back!!!
Hi, I have over 15 years never had very swollen joints, deformed hands arms legs and feet with nodules, painful at the moment. Subsequently I have to have a reversed new joint in my shoulder, which the surgeon said to wait until I can’t stand the pain anymore. I have now developed pain in my lower back. I feel rheumatologist aren’t interested in me, have taken Methatrexate and Steroids with lots of pain killers for years now with no improvement/remission .
Dear Jackie,
If possible in your situation, I’d look for another rheum dr if he/she is not “interested” enough. If you want to try more aggressive treatment (more than one dmard like mtx at a time – triple therapy – OR adding a biological medicine to the mtx), then you should have that option. Just progressing along is not good enough.
I know what it is to just “progress” along & rely on steroids for survival – I’ve been through all the options tho – it doesn’t sound like you have yet.
You are so brave with that shoulder – I pray your surgeon does the right thing at the right time for you.
Never settle. Always fight. Best wishes and prayers for you Jackie.
Hi Everyone,
I believe I have had RA for many years, even as a child. I have always had pain in my joints and especially my knees. I started feeling sick, weakness and fatigue in 1999, however, my doctors gave me the run around, you look fine, maybe you need a tranquilizer. Then I started having positive ANA’s. So I was back and forth to the doctor. In my case, my swelling was transient. I would have 2 swollen, hot, red knees and by the time my appointment came around, my knees were back to normal. My sed rate and RA tests were always negative. In 2014 I began feeling extremely sick, and I had swelling in between my knuckles. A rheumatologist said I might end up having sero negative RA. In 2016 my ankles were so swollen I could not see my ankle bone. My metatarsals were so swollen I could barely walk. My hands and wrists were very swollen, I could barely use my hands. I saw my rheumatologist and she said that it was definitely RA. She said that it did not matter if my CCP or RA came back negative, she said the symmetrical swelling was proof. My question is if I have so much swelling to have a diagnosis, why then do I test negative for RA and CCP? You would think that someone (me) with so much pain and swelling and internal sickness would show something on a lab test. I have spoke to many older women with RA, I can see the disfigurement, but they have never had swelling. They have obvious bone destruction and a positive RA test, but no swelling. My opinion on this is that there are many faces of RA. No one is the same. Since they really do not know what causes RA, how can they determine what kind of symptoms are universal? Until they find the causative factor, then I believe they (the doctors) should be more open in diagnosing this illness.
Dear Rose, thank you for your insightful comments. A few ideas of how this happens: There are multiple versions of CCP or RF and they are not all tested routinely. Labs do make mistakes – I’ve seen it. There are also more antibodies being identified. My study has led me to understand that different symptoms are caused by different cytokines / immune factors, so it is logical that symptoms occur in different combinations over time in a patient – or in different patients. Some have dramatic obvious swelling early – some later – some never do. But there is still pain – or damage or other symptoms. You are so right.
I hope to respond further to your post in a full-length article as soon as I can. So sign up & stay tuned. Best of luck to you.