Preclinical Rheumatoid Disease: There Are No Joints in the Lungs
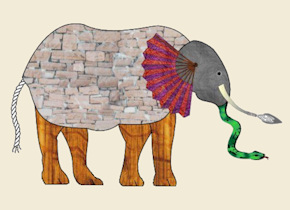 My mom used to read to me John Godfrey Saxe’s 19th century version of a famous Indian legend, The Blind Men and the Elephant. I’m certain it contributed to my zealous love of evidence. Over the last couple of years, interacting with thousands of people with Rheumatoid disease, I came to the conclusion that only certain parts of this elephant were perceptible to those who define and treat the disease. Then, interacting with researchers, I saw that other parts of it are being identified behind the scenes. Today, I can bring you a glimpse of what we’ve witnessed.
My mom used to read to me John Godfrey Saxe’s 19th century version of a famous Indian legend, The Blind Men and the Elephant. I’m certain it contributed to my zealous love of evidence. Over the last couple of years, interacting with thousands of people with Rheumatoid disease, I came to the conclusion that only certain parts of this elephant were perceptible to those who define and treat the disease. Then, interacting with researchers, I saw that other parts of it are being identified behind the scenes. Today, I can bring you a glimpse of what we’ve witnessed.
Bruce Jancin, staff writer for Rheumatology News wrote about one part of that Thursday in Airways Abnormalities May Represent Preclinical Rheumatoid Arthritis.
“Increasing evidence suggests that RA is smoldering in the lungs during this preclinical stage, which can last a decade or more. Indeed, bronchiole-associated lymphoid tissue may actually be the site where tolerance is broken and RA-related autoimmunity and systemic inflammation are generated, according to Dr. William F.C. Rigby, professor of medicine and professor of microbiology and immunology at Dartmouth Medical School, Hanover, N.H…
“‘If methotrexate can be used to prevent the vascular complications of atherosclerosis, why can’t we use it to prevent RA? There is now [a National Institutes of Health] clinical trial proposing this. Because once the joint gets targeted, damage can happen very, very quickly. Many people have erosions on x-ray after only weeks of symptoms,’ the rheumatologist observed.
“He credited the discovery of the existence of a lengthy preclinical seropositive phase of RA to landmark studies involving U.S. military personnel with centrally stored blood samples that were available for many years prior to their being diagnosed with RA (Ann. Rheum. Dis. 2008;67:801-7). The existence of this years-long preclinical lag time has since been confirmed in multiple other populations.” (Emphases added.)
Preclinical RA in research and the real world
One week ago in Houston I had lunch with a patient from Denver explaining that close to her home investigators are studying preclinical RA by locating people with positive antibodies who do not yet have joint symptoms. Families like these want to know whether relatives (twins in this case!) will be affected. I described the strategy to observe what happens with RA before joints are affected. Four days later, we read the RN article.
The Colorado researchers have been screening and conducting interviews with first-degree relatives of RA patients and obtaining blood samples at community health fairs during the past few years learning to identify early RA and preclinical RA. According to Jancin, the earlier Armed Forces study demonstrated that the serologic profile method (anti-CCP and/or two or more rheumatoid factor isotopes) is 96% reliable for identifying RA before inflammatory arthritis is evident. We’ve examined possible triggers to Rheumatoid disease and you can see the advantage of being able to follow people who do not yet have diagnosable RA symptoms.
Airway disease exists prior to inflammatory arthritis symptoms
CT scans showed 77% of 45 preclinical RA patients experienced a form of airway disease. Only 31% of the antibody negative control group showed airway abnormality, but 12 people with early RA (diagnosed less than one year) were similar to the antibody positive pre-RA group.
Significantly, “none of the seropositive preclinical RA subjects with CT lung abnormalities had any evidence of synovitis of their joints on MRI, indicating that RA isn’t smoldering preclinically in their joints for a long time prior to the time they show up in a rheumatologist’s office with joint symptoms.” In order to determine where RA disease begins and how to arrest it, we must look outside the joints as these researchers are. “These findings suggest that the lung may be an early site of autoimmune-related injury, and potentially a site of generation of RA-related autoimmunity. Further studies are needed to define the mechanistic role of lung inflammation in the development of RA” (from abstract for Airways abnormalities and rheumatoid arthritis-related autoantibodies in subjects without arthritis: Early injury or initiating site of autoimmunity?)
Postblog: We’ve known that joints are where Rheumatoid disease ends up, but not likely where the disease begins. My unique vantage point, listening to the voices of so many people with this disease, has compelled me to advocate for research and treatment which considers the entire disease. We have yet to find the sine qua non of Rheumatoid disease. But the future is rapidly arriving when we’ll look at this elephant with our eyes wide open. Or at least each blind man’s voice will be heard.




Very interesting. I had lung problems for at least a decade before being diagnosed with PsA and have only become sero positive for RA 6 years after developing joint symptoms. As my many conditions advance (PsA, RA, ITP, coeliacs etc) I’ve come to realise that I only have one condition, Autoimmune Disease. PsA/RA are only a set of symptoms of a much bigger beast. When I get asked what I have, I now reply Autoimmune Disease.
Cat, that makes sense to me. With my sero-negative RA I also have Fibro. They don’t seem very interested to repeat my RA factor test at any time since I was diagnosed by sono. But have had drs say that since I am sero-negative, I shouldn’t have much disease activity, so less pain. Yet I already have damage to both wrists and two fingers on my right hand, one of which I could use to give that doc a message! It doesn’t bend much anymore as it is. I am genetically linked to Lupus, RA and Fibro by sister and mother. Was really hoping I had dodged the bullet since I was over 50. Got me at 54.
I have recently developed the “mask” when I am really tired or stressed. When I mentioned this to my primary doc, he said it wouldn’t surprise him if I had Lupus, but why bother testing since I am on the medication for it already! I’ll talk to my Rheum doc, think he might have a different view.
Kelly, wonder if this is where smoking being a factor comes in? Makes sense to me that if it smolders in the lungs first, smoking really ticks it off!
Yes I agree. Smoking is a likely culprit to kick off the process in many people through some type of “insult” to the tissue. If a person was not exposed to smoke, then there would have to be a different trigger that kick-started the antibodies to citrillination cycle. There is a link at the bottom of the post to the most recent post on Triggers of RA.
this is so interesting. When I was 22 I had pneumonia and ever since then, every time I catch a cold I end up with severe bronchitis which requires antibiotics, and at least once a year turns into pneumonia. Diagnosed with RA 20 yrs later, after spending a long painful summer of working both night and day at work (i.e. mucho, mucho stress). Now I wonder if my lungs were telling all that time that I was developing RA, and it just took one really bad physically stressing period for it to flare out into diagnosis.
I could’ve written your reply word for word. Same circumstances, same time frame. If only we’d known.
This article describes me to a tee. Started off with one lung nodules, diagnosed with RA, and now have a second nodule…all within 1 year.
Wonderful news for those who are seropositive and asymptomatic. Yet more frustrating news for people like me who are seronegative and wildly symptomatic. I hope someone is conducting research on our reality of RAD.
RA diagnosis 2004. Lung cancer diagnosis 2008. Hummmmmm.
Grew up with second hand smoke. No base line chest x-ray with initial RA dx. Hummmmm.
I have an aunt that suffers from this terrible disease. Please do all you can to support this foundation.
Thank you for such an insightful piece. Glad to see they are looking at the root issues. I worked in a wet chemistry lab for 11 yrs, then onto another lab for seed production. They used a green chemical that improved germination for some products.I went on to work in in animal shelter that had huge issues with their air exchange system, I used to laugh that I got kennel cough like the dogs did. Not so funny when I was diagnosed with RAD during my work there.After forming nodules,fatigue and much pain I resigned, the disease had its grip on me.I also live in area that uses poultry,and hog manure as fertilizer, this manure is laden with compounds that I used to see in the lab.As large operations they must keep the animals on antibiotics so they see less mortality and more profits. When putting this onto the fields the smell is horrendous, but it spews dust particles,or vapor into our air.We are also surrounded by hog lagoons that produce millions of tons of manure and gases.I am not blaming any one issue here,as I was not the best steward of my body, but it makes one wonder what the heck is going on here with so many people, young and old diagnosed with auto immune diseases.
Here is the link on the CDC and what they have found.
http://www.cdc.gov/nceh/ehs/Topics/CAFO.htm
Food for thought…..
The optimal part of SMOLDERING I think is MOLD. Has that been looked at? Going back many years I had severe pneumonia and pleurisy. Long story of Dr telling me I’m not so sick. It took me a year to fully recover. Then after my mother passing, moving, a big break up, work, career change and getting married, wedding,oh and 4 miles from LomaPrieta earth quake….Those are the key points but does not cover it all…We had to move due to the earthquake into a house 1/4 the size. It turned out to be a black mold nite mare! This was before you could do anything like sue the landlords who just treated us like…ya, ya, ya…it’s no big deal. What’s your problem… I do sound like a complainer but I can’t help the truth is what it is.
Excellent post Kelly. Simply more proof that we need more research and a more accurate name of the disease. In Kim’s case she had no earlier indicators of lung issues. She was raised in a non-smoking home and she herself has never smoked. Yet when her joint symptoms started prior to her diagnosis she was also having breathing problems that started around the same time. Eventually her rheum said he thought she had asthma, but he did refer her to a pulmonologist. At her first visit with the pulmonologist he diagnosed her with a lung disease that is caused by her RAD. Maybe this article mentioned here by Kelly actually shows that it’s the lung disease that caused her “RA”.
We are coming to understand that it’s not a hand disease at all but a true systemic disease affecting heart & lungs and any other place it chooses. Emphasis on hands has done us a great disservice ovr the last few decades. And the criteria updated in 2010 still focus on them as do “joint counts.” Making dx an impossibility for many btw who have “larger” joints involved first.
Thanks for adding Kim’s story here.
Hi Kelly, Thanks for the article. Interesting thought that the chest lymph nodes would be a place of the acquired auto-immunity. But then the thymus is right there too. I’ve been reading a lot about immunology lately. Very facinating subject and extremely complex. What the immune system does is truly awesome. I guess that’s why it hurts so much when it identifies the wrong antigens. We’ll crack this nut someday.
p.s. In the article it mentioned RF isotope. I think it should be isotype. Big difference. 🙂
I’ll ck on that typo. We got to get the story straight. This whole thing still amazes me that one very sick girl writing blogs in the middle of the night half asleep has gone as far as it has. But we do have a case that needs to be heard. And I’m not giving up. So here we are.
Great article. Newly diagnosed with RA beginning of this year but the more I learn, I have had precursor symptoms for a long time. Along with various joint issues, I have had pleurisy twice, pneumonia once and was referred to a cardiologist for chest (wall) pain of which was proclaimed “it is not your heart” after echo and stress test completed. So much to learn about this systemic disease. I was sent to a rheumatologist 7 yrs ago after pneumonia, joint pain, and a positive ANA. The rheumatologist at UNC specifically said that it could take 7-10 years for a rheumatologic disease to present itself. Guess what? I was diagnosed at the 7 1/2 yr mark. I feel that that Rheum. fellow suspected that, what now is being published, there are many pre-clinical symptoms prior to the visible joint damage. Ever heard the saying “where there is smoke there is fire?” Alot of us have probably been sending out smoke signals for years.
I have copd and mild emphysema in the top of my lungs and pulmonary fibrosis in the bottom of both my lungs and also a nodule in the left lung. I also have tested positive for RA Factor. My lung Dr said that my Rheumatologist would probably be my best bet to diagnois RA however he said I have fibrymyagia, osto arthritist and degenerative joint disease and that my blood work is probably just a false positive so I am seeking a second opionion from a rheumatologist with more experience. I also have fibrosis on my liver and an irregular thyroid with a nodule. My endometrial lining in my uteris is also more than twice the size it should be and I am having surgerory for that tomorrow. History of fistulas and scattered diverticulitis in my colon and Irritable Bowel Syndrome. I believe it is RA that is the war inside my body. I have quit all the medications I have been prescribed that are only to help with all the pain and not to stop the progression. I am using empowering music and meditation and self hynosis as well as going back to work to get me out of bed. The longer I stay in bed the more I hurt when I get up for at least an hour after I get up. It is very frustrating dealing with specialist after speialist still unable to diagnois all my multiple symtoms as one and begin treating the problem. I truely appreciate arthritist warrior for educating me more about RA and making me feel that I am not alone and that there is some hope. Thank you for caring!!!!
Hi Kelly, I haven’t been officially diagnosed yet but the rheum. dr. said he thought I may have RA. I’m to go back for tests if more than my two toe joints are involved. The Dr. did listen to my lungs and asked me if I had breathing trouble. I thought that was strange but now I see why he asked. I told him ‘no’ but come to think of it, I have developed asthma-like symptoms that I assumed were allergies. The symptoms come in allergy season. I never had allergies until three years ago. Oh, and I am a former smoker (13 years smoke free). Chest x-ray was clear three years ago.
My jaw has also been bothering me a lot lately. Is it RA or just me clenching a lot? I don’t know. I’m doing okay but am confused about all of it really.
Your site has been a learning experience for me! Thank for all the information.
Kelly, Very interesting. I was diagnosed with pulmonary hypertension a couple of years before joint symptoms started with no identified cause. Hmmm, I wonder…
I love the elephant analogy, Kelly! I recently have developed inflammation in my ribs (oh yay). I keep hearing from my rheumy that I present a-typically, but what I keep reading from your blog is lots of folks have the same “a-typical” symptoms. Is it us that is reacting differently, or different forms of the disease? I don’t know the answers, but I know keeping myself appraised of knowledge about my elephant, especially from your blog, has helped me in the feeding and care of the thing. One of these days my rheumy might listen to me when I say, um yes, well I learned that from RA Warrior, tyvm. Awesome resource. You might want to try it some time!
As far as the precursor of a lung issue, I didn’t have that myself, but it is always interesting to hear about different avenues of thought and research. As long as we are bringing light to the darkness, let us keep lighting candles until we can see this darn elephant (or the herd of them) clearly.
Jennifer
Thank your your work. This new is fascinating to me, since I have had chronic lung infections for about 10 years before finally nearly dying and having surgery to “fix” my lungs, scraping infection off them ” removing parts. It was a year after the surgery that I was diagnosed with RA, but the major pain of RA began immidiately after surgyer. I just thought it was part of recovery to have my whole body ache. Anyway, the doctors have talked about the trauma of my illness triggering RA. But, maybe the RA was causing the illness all along.
Bang! Another reason I can tell my sons why it isnt smart to even to start smoking or using tobacco in any form…We already knew that smoking was a risk factor, but this gives me pause to think, it is even more ammunition to shoot the nicotine products out of their hands. 🙂
I was wondering too, Megan. Like how does this apply to seroneg? I guess time will tell. Do you have issues with your lungs? I have since I was 17, but there is nothing to hear or see. Joint wise, it seems to be all of them (but nothing on xray unless the latest of the feet show something). Jaw, ribs as well as the main ones. Voice box bothers me even and I’ve been tested lots and scanned for thyroid issues (runs in family). No answers for me. Why is my heart rate too high? Nobody knows. The feet/toes are my worst joints right now. And my shoulders and wrists…. Also it mentions mtx. I just maxed out according to my doc.
I think the Rf antibody usually does show up eventually. But I’ve assumed they will find another type of antibody present in those who do not have Rf. More research… It is similar the question of why mtx can almost completely suppress the disease of some while providing very little relief to others.
Interesting research. My mother has developed lung issues along with nodes the last few years. In November she rapidly lost her sight due to Cornea ulcers. Her eyes have always been healthy. She had her annual eye exam just two weeks before and all was fine. Since it hit both eyes within days and the eyes are not healing properly, they now suspect RA. She has multiple joint problems but no one ever tested for RA till now.
I was diagnosed this past June and am sero-negative. The MVP joints in my hands were hit symmetrically one by one over a week. Then my feet. Six years ago I was hit by sudden muscle weakness. They never figured out the cause and I wonder if that’s when it all started. Two years ago I developed chronic hives. My doctor actually started thinking about RA after all my joint pain disappeared after I was given IV steroids for the hives.
Now my younger sister is struggling with joint pain in her hands. She has had breathing issues for years. Her rheumy appointment isn’t till next month. Knowing I am sero-negative is helpful for her.
We were all exposed to silica dust while living in Cairo. We thought the dust that collected daily on our furniture was sand but recently learned itwas silica dust from an unregulated silica mine near our building. Plus Cairo was very polluted at that time.
Ofc I mean MCP joints not MVP…smile. Sometimes autocorrect is a nuisance.
Very interesting information here. I wonder, though, what ramifications this can have on JRA. I’ve had it since I was five and also suffer from asthma, but the symptoms of both essentially hit at the same time. I know children who have been diagnosed as early as 3 months.
I love that this information is coming about and might be able to lead to preventative, but for many children I’m not sure this will help – especially those in households like mine growing up where you didn’t see a doctor unless something was terribly wrong because there was no insurance… and my family all thinks they’re smart enough to be doctors.
I grew up in a smokers household (never smoked myself) so was constantly exposed to second-hand smoke in the home, in the car, wherever my father went. My father died from vascular disease and dementia after being a lifelong, heavy smoker. My brothers got asthma, I got autoimmune disease (RA, Hashimotos, Fibro).
If ever there was a reason not to smoke this is it: as much as a smoker may choose to smoke and do damage to themselves, they do so much damage to the people around them and the realities of that don’t show up until much, much later.
I grew up with lots of smoke too Betty. Parents and grandparents. Teachers & neighbors. I remember complaining about it.
Wow, Ra came on with a vengeance after a bout of pneumonia. I keep telling my doctor that was the trigger. Thank you for the information
I developed intermittent inflammatory arthritis (which can precede RA) shortly after getting a flu shot during the H1N1 scare. Six months later I had full blown RA. Looking back, though, I realize that it started much earlier – when I had the flu about 5 years earlier. It left me with a horrible cough that lasted for 3 months. After that, every time I caught a cold I ended up with a cough that lasted for months. I believe that the flu triggered my immune system problems and that the flu shot was the final trigger. Now that I am being treated for RA, I have not gotten a terrible cough after catching a cold. Oh, and both of my parents smoked throughout my childhood.
OMG! I had chronic bronchitis and lung problems for nearly 4 decades before I was diagnosed with RA! Symptoms started 33 years ago in my feet, but I remained seronegative until 2006, when I was diagnosed with RA, based on RA-factor, elevated CRP, elevated ESR, and an MRI of my knee which showed joint destruction. In the same month, I also had an MRI of my lumbar spine which showed degenerative disc disease in 4 discs. So, I probably had been harboring Autoimmune Disease in my body all those years. It’s interesting, now, looking back, that since starting on MTX I have not had a single episode of bronchitis or any lung problems. Hmmmmmm! What, exactly, are we treating here: lungs, joints, or an Autoimmune Disease that affects many tissues?
Kelly, thank you for being on the forefront of information gathering and sharing for Rheumatoid Autoimmune Disease! You are a true friend of every person who has RAD.
I have to echo Turtlemom. Kelly, you do incredible things for the RAD community. I don’t even look anything up on the internet any more, know I can find whatever info I need right here. thank you so much!
This is just one more thing that we can identify with. I have never had lung issues even tho I was a smoker for many years until I had back surgery in 2004. I quit smoking, had the surgery and one month later I am flat on my back on a couch for 30 days, strict bed rest. Evidently I had encountered someone with pneumonia. Pleurisy meant I couldn’t sleep in my bed, just didn’t figure that out for a miserable night. Messed me up on my PT, have lingering effects even now. Haven’t had pneumonia since, but have had pleurisy several times since my RAD diagnosis. Even tho my old Rheum doc said it isn’t possible.
One of the first symptoms that I noticed along with joint pain was shortness of breath. I sometimes cannot finish a sentence without becoming short of breath. ER evaluation initially said congestive heart failure. That was ruled out with a stress test and an EKG. I was later sent to have a lung capacity test which came back normal. I still have shortness of breath. The least bit of exertion causes it–even bending over.
Bev, a lung capacity test or a pulmonary function test? My wife had the pulmonary function test, which she failed. That was followed up with a visit to the pulmonologist and even though her rheum thought she had asthma, the pulmonologist diagnosed her with bronchialitis obliterans, a extra articular disease because of her RAD. Through it all, her lungs have been clear and she sounds fine breathing at rest, but under any exertion she became short of breath. Her lung capacity was fine, but her ability to breathe was not.
Eric, I think it was a lung capacity test which I thought for sure I would fail, but I didn’t. This is the first I have heard of having shortness of breath associated with RA. I have not even mentioned it to my rheumatologist. Thank you so much for that information. I will definitely mention it to my dr.
My lungs were also affected from an early age (smokers in home all my childhood/teenage yrs and never smoked myself). Intermittent rib and chest pain when breathing, have vocal cord dysfunction and asthma (well maintained thanks to Singulair). Every joint is involved, even my jaws and cervical spine. Praying for relief and so thankful for Kelly who is our voice and also so thankful for this awesome RAD community Kelly provided a gathering place for 🙂
I was diagnosed with RA in November 2010 and pulmonary fibrosis in March 2011 which the doctors say was brought on by the RA. I also have hypothyroidism. I’ve had croup, bronchitis and pneumonia since I was a baby so I’m sure that played an important role in my lung issues. I’ve had a chronic cough for 8 years and 2 years ago was told that I had fluid in the lower part of the left lung. My son was killed on Easter 3 years ago so I believe that was the stress factor that triggered the RA. My life has completely changed. Had to stop working, don’t have alot of strength to do anything, on oxygen 24/7 – not the retirement I had hoped for.
I was diagnosed with RA 21 years ago . It has been a nightmare at times
I have 2 spinal fusions an ankle fusion a total
Knee replacement that ended up being removed
External fixatit’s and know it’s a flail bone on bone
Fusion. I learned never give up… Hard as it is
Use those functional joints. I also learned to control
My pain. I use a relaxation technique. I sply
Place music on a portable CD. I mentally envision
A favorite place I enjoy. I do take pain meds . I have
A wheelchair I have to use.
I developed a chronic cough after having a flu in 2004. I coughed until I threw up and my eyes hemorraged.
Multiple specialists later, I finally had a Nissen Fundoplication in Jan. 2012 due to a hiatal hernia and micr-aspiration of stomach acid into my lungs – GERD-induced asthma without a single episode of heartburn. I was so excited about the surgery and getting my life back after 7 years of this – a few weeks out, joint swelling and pain began. At first, it was thought to be a delayed reaction to medicines from the surgery, then thought to be a reaction to a new inhaler. Turns out it is RA.
I was a smoker for much of my adult life (embarrassed to say)and began quitting in 1992 – took me until 2005 for it to stick for more than a year. I actually was a nonsmoker during those years more than a smoker – how I wish I’d never started. How I wish someone had figured out what was wrong in 2004 instead of 2012 – perhaps I wouldn’t have RA today. Haunting.
I have RA, endometriosis and some recurring bowel issues which I am sure are all related. I was very interested to read this post about lung issues though as I have also had surgery to remove a fungal nodule from my lung. I developed RA in late 2007. The following year I had a routine chest x-ray while attempting to get onto a clinical trial for RA. That showed a lump in my lung about 2cm wide. Of course everybody immediately suspected cancer although RA nodules were also considered. Numerous scans and a biopsy through the ribs directly into the lump all showed mixed results between negative for malignancy, inconculsive and suspected postive for malignancy. I had the surgery to remove it within weeks and they ruled out cancer straight away but it took nearly another week to work out what it was. It turned out to be a fungal infection called Cryptococcis. It is mainly found in Aids patients but occasionally in others with auto-immune issues. The fungus is found in the environment in things like mould, bird droppings and garden mulch and most people will breath it in and out without any problems. However, occasionally, the fungus gets trapped in the lung. It may stay there forever without developing any further but it can also be triggered into spreading and can spead to the spinal fluid and into the brain and be potentially fatal. In my case I was so lucky that a random x-ray picked it up as I had no other symptoms. It has been completely removed but there is always the potential for it to come back so I take an anti-fungal tablet every single tablet. My worry now is that the biologic drug I need to manage my RA may also lessen the effectiveness of the anti-fungal tablet and allow the fungus to return. There is no test for it either. Anyway, the reason I’ve mentioned all this here is that there is no way of knowing which came first, the RA or the Cryptococcosis (or the endo for that matter). There is not much research that I can find about the connection between these two diseases other than this article. http://chestjournal.chestpubs.org/content/115/3/610.full.html I’d be interested to know if anyone else has had any experience of this disease.
Someone recently gave me some Ganoderma Coffee. Anyone know anything about using this mushroom? I need to know the effects it may have with Methotrexate or my immune system? They also say it helps support liver function. I always am ver wary of this supplements. My Doc dismisses anything that doesn’t have FDA approval so I am not even going to bother her with my questions!
I have had RA for 14 years. It showed up not too long after a lung cancer scare which turned out to be an abcess (treated with megadose of antibiotic for six months. Subsequently began experiencing RA symtoms and was started on Remicade and Methtrexate. I considered the drugs to be a lifesaver. Now, all these years later, I am going through another diagnostic nightmare where the doctors cannot determine whether I have cancer or rheumatoid lung. No Remicade or Methotrexate since May, only low dose Prednisone, so lots of joint pain. I am truly afraid that the Remicade may have been to blame, but I can’t function without it.
Wow, after reading “Preclinical RA disease” I was blown away. I am 59 years old and I was only diagnosed 1 year ago with RA. The catch is I had my right lung collapse when I was 42. I also had to flares that the RA doctor thought might be Lupus, but nothing ever showed on a blood test. About 4 years later I developed fluid in my lung. Again no one mentioned RA. Three years ago I kept having shortened breath and major fatigue, again it took 2 years to finally get a diagnosis of RA. I wish I had been able to get on the methotrexate a long time ago.
Learning so much from RA warrior, Kelly! Gentle hugs for you. I keep getting these ahas! I have had bronchial problems since my early 20s. Have been hospitalized w/pneumonia several times, nearly dying twice. In one hospital I got Mrsa, so I have outbreaks of that wretched infection from time to time. I was a social smoker from age 14-50, when I finally decided breathing was preferable. But now at 74, I find I’m short of breath all the time.’infer winded taking the trash out! I have a referral to see a pulmonary specialist, so I’ll add him to my long list of medical professionals, none of whom who confer w/the others unless I specifically request it each time. I am going to start saying I have RAID, rheumatoid auto immune disease. Gotta go lie down now.
Diagnosed with psa two years after plural effusion still a scar in lower lobe of lung so this does make me wonder thanks Steve.B
I am so thankful to have found this website. I was just diagnosed in Feb with RA but have had multiple systemic inflammatory symptoms for 30 years. The lung issues were always the returning symptom that would improve with steroids. I always knew that all of my “itisis” we’re caused by an auto-immune disorder but could never get an accurate diagnosis so I just gave up trying. I was finally diagnosed this year because of major joint damage in my foot which led to surgery and a referral to a rheumatologist. Finally this time my lab tests were positive for RA. I can so relate to all of your posts.
I was diagnosed with pulmonary fibrosis in April of 2013 and then shortly after with RA. I was told the ISD was probably the beginning of my RA. Currently I am having tachycardia issues so was sent to cardiology – have no results yet but the suspicion is pulmonary hypertension. We will see.
I have recently added my experience with RA and Fibrosis to RA Warrior and am confused. My RA diagnosis was made in 1973. My Pulmonary Fibrosis Diagnosis was made in June of 2014 by accident. I have no symptoms yet. The mild to moderate scarring was found on a CT Scan while checking for an enlarged heart. My Drs. tell me the Fibrosis is either a side effect of RA or of the years of Methotrexate I have taken. Needless to say I am more than confused.
I am just wondering the obvious question: how should lung disease eg. bronchiectasis and rhuematoid arthritis be treated. I believe my disease smoldered for years too. Doc is reluctant to give DMARDS other than anti malarials because of lungs, pain continues..right course?
Pingback: Our Friend Died from Rheumatoid Disease | Handicap Accommodations
I became effected after being exposed to black mold also.
My RA started with my lungs. I started with chest pain, and cough that I had for 7 months. My primary care doctor keep saying I had bronchitis. Then it went from being bronchitis to a pneumonia that wouldn’t resolve by using antibiotics. After 7 months, the pain, swelling and stiffness occurred in my hands, feet and knees. It was to the point that I couldn’t walk without crutches. I went to the emergency room and was in the hospital for two weeks. After being on 9 different antibiotics that didn’t help my breathing or the so called pneumonia, I was given breathing assessments, and x-rays which showed that I was only using 10 of my right lung. A biopsy confirmed the inflammation in my right lung. The doctor decided to give me steroids through IV. I could breath fine and was walking within a day without crutches. A day or so later I was diagnosed with RA and Interstitial Lung disease. That was 5 years ago. Since then I have had two major flares that caused me to be hospitalized and my lungs were always effected. This article provides good information. Thanks
I was diagnosed with RD in 2001. The first time I knew there was something wrong with me was in the 80’s. I was numb on the left side from head to toe and fatigued easily. I was told I was hyperventilating by one doctor. I was checked for MS and carpal tunnel. When I went on Orencia in 2010, the numbness ended as did a lot of my fatigue and pain . Up to that point, I had been on 12-13 different meds for RD, several biologics with unsatisfying results. However,I have had pressure and pain in my chest for a long time. It’s not the heart. I am having a chest CT this afternoon. Around the same time I was diagnosis with RD, I was diagnosis with asthma. I have been diagnose with IBS. Seems everything comes back to the autoimmune. Thanks for this blog; it has helped so much. It can be a lonely experience.