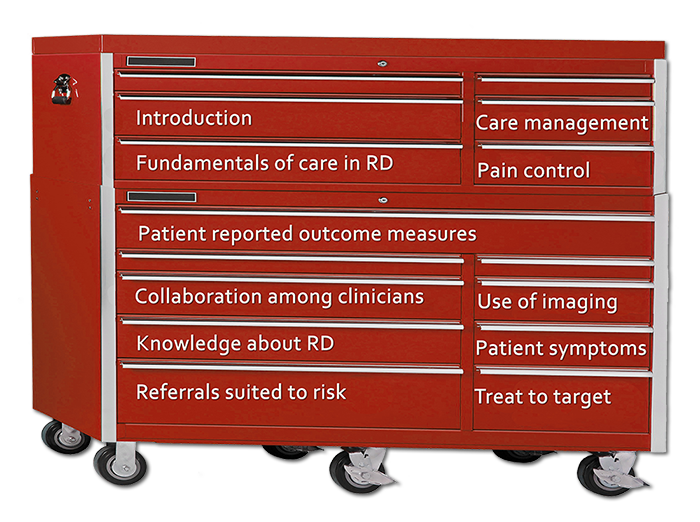
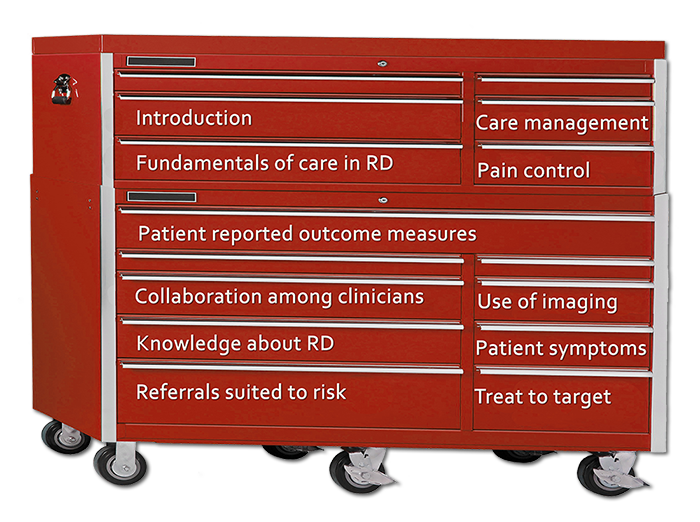
Mouse over the labels on the Tool Chest below to see topics important in health care for people with Rheumatoid Disease (RD) / Rheumatoid Arthritis (RA). Click to read each section of the toolbox. Clicking the small red toolbox takes you to an index of topics.
Welcome to the RA Care Toolbox
Guidance for medical professionals treating people with Rheumatoid Disease
If you’re a professional who treats people with Rheumatoid Disease (PRD), you have an extraordinary mission. You have an opportunity to help people with a disease that is challenging to manage because it is complex and not yet well understood. RA Warrior has educated patients for several years about ways to improve their health and pursue adequate treatment. The purpose of this tool is to educate healthcare professionals about the most critical elements of care in RD and answer important questions I’ve been asked: “WHAT DO PATIENTS WANT DOCTORS (OR NURSES…) TO KNOW? How can we do a better job caring for people with RA?”
The purpose of this toolbox is to provide healthcare professionals with a better understanding of the medical needs of PRD. This resource will reference professional guidelines, expert recommendations, and patient feedback about the treatment of PRD. As current research is expanding knowledge about RD, there is a need for both patients and healthcare professionals to be up-to-date. Please check back as these pages are updated or expanded.
Rheumatoid Disease (RD) or Rheumatoid Arthritis (RA) is a systemic immune-mediated disease that can affect any part of the body. In RD, excess immune activity causes inflammation that usually leads to fatigue, fever, stiffness, or a feeling of being ill. Typically, RD attacks the musculoskeletal system, causing joints or tendons to become painful, swollen, or weak, and leading to disability or permanent damage. The disease can also lead to problems with various organs or systems, including the circulatory or nervous systems, eyes, skin, bones, heart, or lungs. Click here to read more information about RD.
Like patients with other complex chronic diseases such as Type 1 Diabetes, persons living with Rheumatoid Disease (PRD) often require regular care or continuing support from medical professionals. This often necessitates consultation with various medical specialists and use of multiple prescription medications. The complexity of RD and a lack of familiarity in the medical community with its comprehensive nature contribute to the immense challenge of treating RD.
This tool includes 10 ways to provide good care for PRD listed on the tool chest, plus several other sections listed in the box below.
MORE TOOLS TO PROMOTE EXCELLENT CARE TO PEOPLE WITH RHEUMATOID DISEASE
Summary of fundamentals of care in Rheumatoid Disease
Levels of treatment response in Rheumatoid Disease
Drug side effects in Rheumatoid Disease: How to help
Shared decision-making and Rheumatoid Disease
What NOT to do
Key facts & info on Rheumatoid Disease
 1. ATTENDING TO FUNDAMENTALS OF CARE IN RD
1. ATTENDING TO FUNDAMENTALS OF CARE IN RD
It is imperative that you understand the fundamentals of care in RD, and remain aware of updates in care recommendations based on current research. Investigators found recently that recommendations for treatment of PRD have not substantially impacted patient care: “Publication of the recommendations did not significantly change treatment patterns for those with active disease… Substantial numbers of RA patients with active disease did not receive care consistent with the current ACR treatment recommendations. Innovative approaches to improve care are necessary.”[7]
Fundamentals of care for RD include
- Physically examining patient’s joints
- Discussing symptoms that are described by patient
- Evaluating treatment plan according to current professional guidelines
- Informing patient of current treatment plan
- Inquiring of patient whether pain control is adequate
- Administration of immunizations recommended by guidelines
- Regular review of systemic symptoms, referring patient as necessary for tests or specialty care
- Referral for physical therapy, specialty care or surgical evaluation of joints, including spine, jaw, and sacroiliac joints
- Inquiring whether assistance with disability documentation is necessary
CLICK HERE FOR MORE COMPLETE SUMMARY OF FUNDAMENTALS OF CARE IN RD
Read more about the fundamentals of care in RD
- Significant Numbers of RA Patients Don’t Receive Recommended Care
- If the Gloves Come Off, We Might See the Irony of Rheumatoid Disease
- The 10 Fundamentals of Care for Rheumatoid Patients
- A Paradigm Shift in Rheumatoid Arthritis Disease Activity? Part 1
- EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs
- ACR Practice Guidelines for Rheumatoid Arthritis
- British Society for Rheumatology and British Health Professionals in Rheumatology Guideline for the Management of Rheumatoid Arthritis
- Rheumatoid Arthritis: Current Diagnosis and Treatment Practices (Mayo Clinic)
 2. MANAGING CARE IN RHEUMATOID DISEASE (RD)
2. MANAGING CARE IN RHEUMATOID DISEASE (RD)
RD can affect many different aspects of a patient’s health and carries several serious health risks. The disease can affect vital organs in several ways and its systemic inflammatory nature is a burden on a patient’s health generally. Also, PRD are more likely to experience several co-morbid conditions.
It has been known since at least the year 2003 that PRD do not receive optimal health maintenance or adequate preventive care services.[2] Actually, PRD tend to receive preventive care or risk management even less frequently than the general population or those with other chronic diseases for various reasons.[3, 4] The American College of Rheumatology has published a position statement which supports rheumatologists as principle care physicians for people with rheumatic diseases.[5] While a shortage of such specialists makes that unlikely, it indicates the nature of the responsibility a rheumatology specialist has in assisting PRD to obtain adequate attention for RD.
One key factor to obtaining appropriate care is to maintain a problem list. A problem list must be maintained for PRD because they are likely to have multiple, chronic, complex health issues.[6] If you are not doing so, ask who is managing care for this person or maintaining a complete problem list in order to determine whether at least the minimum level of care is being performed. If no one has created a problem list, assist the patient in doing so.
Read more about adequate RD care management
- Can We Treat the Whole Person or at Least the Whole Disease?
- Why Rheumatoid Disease Patients Still Fall through the Cracks
- Where the Rubber Meets the Road or What If Only the Cancer in Dave’s Kidneys Was Treated?
- Secondary Sjogren’s Syndrome and Rheumatoid Arthritis: a Primary Problem
- Rheumatoid Arthritis Muscle Wasting: Rheumatoid Cachexia
- Recognizing the Anguish of Depression in Time for Help
 3. ADDRESSING RHEUMATOID DISEASE (RD) PAIN
3. ADDRESSING RHEUMATOID DISEASE (RD) PAIN
Most RD symptoms are what patients call “invisible,” having no visible evidence that others can readily detect. In light of what is now known about Rheumatoid disease activity distinguished by imaging (see #7 Imaging) and the ongoing damage related to it, patient reports of Rheumatoid Disease-related pain should be given credence.
Rheumatoid Disease is well known to cause intense radiating pain.[14] In spite of disease treatment, about three-fourths of PRD still survive on daily doses of anti-inflammatory medicines and pain medications.[15] In a large survey, 68% of PRD reported having zero pain-free days each month, 31% reported moderate to severe pain at least 15 days in an average month, and on average, they experienced only two pain-free days per month.[16]
Disease-related pain must be adequately addressed in conjunction with disease care. If for some reason, you are unable to provide satisfactory pain care, you should assist patients in finding that care from another professional.
If the severe or prolonged pain of RD is untreated, consequences include not only the patient’s suffering but also risks from comorbid conditions. The severe pain of RD can mask other serious health problems such as cancer or heart disease. PRD become accustomed to daily pain, and tend to ignore symptoms that would cause most people to seek help, a likely contributor to increased silent, unrecognized heart attacks and sudden cardiac deaths in PRD.[17, 18]
Read more about RD pain
- IOM Pain Report Relieving Pain in America Gets Mixed Reviews
- RA Reality Versus “The Lie”
- Should Chronic Pain Patients Be Treated in the ER?
- Patient’s Rebuttal to RA Pain Catastrophizing Claims
- Does Rheumatoid Arthritis Pain Really Hurt That Much?
- It’s Just Pain, Right? No, Dr. No, It’s Not
- Rheumatoid Arthritis Pain
 4. USING PATIENT REPORTED OUTCOME MEASURES
4. USING PATIENT REPORTED OUTCOME MEASURES
Use patient-reported outcome measures (PRO’s) to help gauge disease activity, specific disease-related problems, and disease impact on a patient’s life overall. Patient reported outcomes help reduce discrepancies between patient and clinician estimation of disease activity. Data generated from patient self-reports is often more accurate and complete, making it a useful tool to bridge a communication gap.
In spite of a large body of research demonstrating the value of PRO’s in rheumatology care, only about 20% of those providing usual rheumatology care incorporate PRO’s into patient care.[1] PRO’s are sometimes administered merely to satisfy a directive set by a payer or a governing body. However, if PRO’s are administered, but not properly utilized, they will not improve care and communication. PRO’s can be administered in the waiting room and scored in less than a minute.
Read more about patient-reported outcome measures
- Would Relying on Patient Generated Data Make a Difference?
- The Value of Patient Reported Outcome Measures of Rheumatoid Arthritis
- Weight of Patient Reported Outcome Measures on Diagnosis & Treatment of RA
- The HAQ’s, the RAPID’s & the Rest: 3 Reasons It’s a Moot Point
 5. COLLABORATING WITH OTHER PROFESSIONALS
5. COLLABORATING WITH OTHER PROFESSIONALS
It is crucial that you facilitate cooperation between your practice and other physicians. People with Rheumatoid Disease (PRD) will likely need the advice of several physicians including a general physician, an ophthalmologist, a podiatrist, a physical therapist, and an orthopedist. Often, it is also necessary for PRD to consult a cardiologist, pulmonologist, neurologist, or sometimes a psychotherapist, massage or acupuncture therapist, or a pain specialist. In addition, a PRD may need to consult a disability attorney as well as a pharmacy, laboratory, infusion center and a radiology facility.
When appropriate, rheumatology specialists should refer patients to other specialists to ensure their adequate care. Assisting your patient with the process of coordination of care is fundamental to her long-term health. Records and recommendations related to the patient’s rheumatoid disease should be communicated to interested parties, in light of guidelines and known risks for PRD, but it is also critical that a rheumatology specialist include exchanged information in evaluation of a patient’s Rheumatoid Disease.
Read more about how physician collaboration benefits rheumatoid patients
- Do you have a Rheumatology Care Team?
- Where the Rubber Meets the Road or What If Only the Cancer in Dave’s Kidneys Was Treated?
- Recognizing the Anguish of Depression in Time for Help
- Secondary Sjogren’s Syndrome and Rheumatoid Arthritis: a Primary Problem
- Ciprofloxacin / Fluoroquinolone Tendon Dangers with Rheumatoid Arthritis
- Does Rheumatoid Arthritis Affect Tendons?
- 20 Facts About Rheumatoid Heart Disease
- From The Rheumatologist: It Takes All Kinds: A look at the rheumatology practice team
 6. EXPANDING KNOWLEDGE OF RHEUMATOID DISEASE (RD)
6. EXPANDING KNOWLEDGE OF RHEUMATOID DISEASE (RD)
Educate yourself about this disease as much as possible, including allowing patients to educate you about their experiences with it. Bear in mind that not enough is known about RD, so intellectual curiosity is a great advantage. Recognize that information in textbooks may be outdated, incomplete, or mistaken about some aspects of RD.
A more comprehensive perspective is needed with regard to the disease and the ways it affects patients’ health so that diagnosis can occur earlier and treatment can be more successful. A broader view is also needed with regard to musculoskeletal symptoms. For example, disease activity in joints is not limited to synovitis, and significant damage is not limited to bone erosion. Rather cartilage loss and tenosynovitis are significant aspects of disease activity.[8, 9]
To keep learning about RD
- Stay current on peer-reviewed research, and specialty guidelines.
- Remember that advertisements and drug “reps” present only one point of view of the disease or its treatments.
- Encourage your patients to be well informed about the disease and its treatments.
- Be willing to read new research, even when it’s provided to you by patients.
- Attend scientific meetings such as EULAR and ACR.
- Read about patient experiences online in public forums such as blogs and social media.
Read more about Rheumatoid Disease
- A Paradigm Shift in Rheumatoid Arthritis Disease Activity? Part 2
- 20 Rheumatoid Arthritis Patient Facts I learned from RA Patients
- A Paradigm Shift in Rheumatoid Arthritis Disease Activity? Part 1
- 620 patients tell their first symptom of RD – hands are not a majority
- 10 Common Rheumatoid Arthritis Myths
- 10 Key points on RA
- The Immune Fingerprint and Rheumatoid Disease
 7. EFFECTIVELY USING TOOLS FOR IMAGING
7. EFFECTIVELY USING TOOLS FOR IMAGING
Often Rheumatoid Disease activity is not obvious to the naked eye until after permanent damage has occurred or led to deformity. For decades it has been known that x-rays are ineffective for judging disease activity. However, imaging tools such as musculoskeletal ultrasound (MSUS), magnetic resonance imaging (MRI), computed tomography (CT) scans, and nuclear bone scans (scintigraphy) are available to provide more information when clinicians are uncertain of disease activity.
In 2006, Brown et al. demonstrated by MSUS and MRI that synovitis is persistent in 96% of patients judged by clinicians to be in clinical remission, based on blood tests and lack of external swelling in their estimation.[10] Studies have continued to provide evidence that MSUS detects disease activity that clinicians otherwise fail to recognize.[11] In 2013, EULAR published ten specific recommendations for the role of imaging in the management of RA.[12] “’You can see raging inflammation in joints that are not swollen or tender,’ he said in an interview. The discrepancy between clinical symptoms and the ultrasound appearance can be ‘surprising,’ said Dr. Kelly, a rheumatologist at Mile End Hospital in Barts Health NHS Trust in London,” who presented a study on MSUS at EULAR in 2013.[13]
Cost has prohibited routine use of imaging except MSUS, which is not available to most patients in the U.S. because few are trained to use MSUS for diagnostic purposes. Because of its value not only in detecting disease activity, but also promoting earlier diagnosis, MSUS training should be emphasized in both radiology and rheumatology.
In light of growing evidence that Rheumatoid disease activity is not always apparent to the clinician’s eye, patient-reported outcomes should be given significant weight when evaluating Rheumatoid disease activity; patients are typically aware of symptoms that indicate disease activity. Whenever possible, clinicians should seek expert training in diagnostic use of MSUS, or refer their patients to a trusted colleague for MSUS evaluation if disease activity is in doubt. Failure to treat a PRD due to lack of conspicuous external swelling can have devastating consequences.
Read more about imaging for Rheumatoid Disease
- 10 Reasons We Might Want a Musculoskeletal Ultrasound (MSUS) of a Joint
- Rheumatoid Arthritis Swelling, Take Two
- Stand-up MRI and 6 More Useful Things to Know about Imaging
- Measuring Rheumatoid Arthritis Disease Activity
- Nuclear Bone Scans for Rheumatoid Arthritis or Scintigraphy
- 2 Reasons Monitoring Rheumatoid Arthritis Matters
- ACR report on the use of musculoskeletal ultrasound in clinical practice
- EULAR recommendations for the use of imaging in the management of Rheumatoid Arthritis
- The evolution of ultrasound in rheumatology, in Therapeutic Advances in Musculoskeletal Disease
- More RAW articles on musculoskeletal ultrasound (MSUS)
 8.RECOGNIZING THE IMPORTANCE AND UNIQUENESS OF SYMPTOMS IN PRD
8.RECOGNIZING THE IMPORTANCE AND UNIQUENESS OF SYMPTOMS IN PRD
Be aware of symptoms experienced by a particular person with Rheumatoid Disease (PRD). At each visit, inquire about symptoms, without dismissing unexpected or discreet symptoms. Accept a list of current symptoms if submitted by a patient, or an electronic app used by a patient to record symptoms.
Since RD is a systemic disease like Lupus or Multiple sclerosis (MS) symptoms may be significantly reflected in various organs or body systems, or the patient’s general health, as well as the musculoskeletal system. Unfortunately, many short descriptions of RD are inadequate, even those obtained from medical textbooks. Numerous misconceptions have persisted even after evidence has disproven them.
Common misconceptions about RD symptoms:
- That RD does not affect the spine.
- That conspicuous swelling always accompanies disease activity.
- That stiffness usually occurs in the morning, i.e. “morning stiffness.”
- That all patients flare periodically. In reality, many live in a state of persistent disease activity.
- That vocal cord involvement is rare in RD.
- That RD does not usually affect DIP joints.
- That hands are affected first or worst, or provide a gauge for disease progression.
- That extra-articular symptoms are uncommon.
- That fatigue is always a result of side effects, lack of sleep, or response to pain.
Read more about RD symptoms experienced by patients
- Livedo reticularis diagnosis – she knelt next to me with a medical textbook
- Does Rheumatoid Arthritis Affect Tendons?
- Does It Matter Whether Rheumatoid Arthritis Affects DIP Joints?
- What Is it Like to Have Rheumatoid Arthritis? Part 1: The Usage Principle
- Poll Shows Textbooks Wrong on Rheumatoid Arthritis Morning Stiffness
- 7 Atypical Rheumatoid Arthritis Effects Are Actually Typical
- What Is Crepitus in Rheumatoid Arthritis / Disease?
- Rheumatoid Arthritis Fevers
- Rheumatoid Arthritis Swelling, Take Two
- A Paradigm Shift in Rheumatoid Arthritis Disease Activity? Part 1
- 20 Rheumatoid Arthritis Patient Facts I learned from RA Patients
- It’s Simple: Who Gets Dactylitis or “Sausage finger”?
- Dozens of articles on RD symptoms with thousands of comments by patients
 9. REFERRING TO SPECIALISTS
9. REFERRING TO SPECIALISTS
Like other chronic systemic diseases including Lupus, Multiple Sclerosis, and Type 1 diabetes, Rheumatoid Disease (RD) can require the advice and treatment of multiple medical specialties. People living with Rheumatoid Disease (PRD) manage many symptoms related to the effects of the disease itself, or its common comorbidities. (See also #5 Collaborating with other professionals).
Referrals to other clinicians should be made for baseline evaluations according to common susceptibilities for PRD such as eye problems, heart or lung disease, and spine-related problems. As patients report symptoms such as shortness of breath, neuropathy, rashes, vascular abnormalities, digestive problems or pain, falling, dropping things, or issues that concern them, they should be referred to an appropriate specialist for evaluation. There is evidence that both patients and clinicians tend to underestimate risks related to RD that may impact the long-term health of PRD.
Read more about extra-articular Rheumatoid Disease
- Where the Rubber Meets the Road or What If Only the Cancer in Dave’s Kidneys Was Treated?
- Why Rheumatoid Disease Patients Still Fall through the Cracks
- Secondary Sjogren’s Syndrome and Rheumatoid Arthritis: a Primary Problem
- Can We Treat the Whole Person or at Least the Whole Disease?
- 5 Reasons Rheumatoid Disease Is a Better Term than Rheumatoid Arthritis
- Preclinical Rheumatoid Disease: There Are No Joints in the Lungs
 10. TREATING TO TARGET IN RD
10. TREATING TO TARGET IN RD
Early and aggressive treatment has been shown in clinical studies to produce the best outcomes for RA patients.[19, 20] In order for disease activity (DA) to be suppressed aggressively, it must be measured. Treat to target (T2T) is an approach to treating RD that combines aggressive treatment, regular monitoring of DA, and the setting of a goal (the “target.”) T2T is similar to the model of tight control in diabetes, and has been shown in studies to result in lower DA levels, which means less pain, disability, and damage for PRD.
According to the TICORA, a pioneering study in T2T in Rheumatoid Arthritis, “Present treatment strategies for rheumatoid arthritis include use of disease-modifying antirheumatic drugs, but a minority of patients achieve a good response.”[21] PRD respond differently to medications, but few experience an immediate or complete response. However, as TICORA and other studies demonstrated, striving for a specific improvement target improves outcomes.
Experts agree the ideal target is remission, which experts have defined this way: “the absence of signs and symptoms of significant inflammatory disease activity.”[22] But, remission and “low disease activity” have different definitions according to various DA tools, other than “symptom-free.” In T2T, disease activity is measured, and if it is not improved, the treatment plan is adjusted. An expert international task force recommended that drug therapy be adjusted at least every 3 months until the desired target is reached.[22]
Read more about treating to target
- Rheumatoid Arthritis (RA) Treat to Target
- 2 Reasons Monitoring Rheumatoid Arthritis Matters
- What about a Clinical Protocol for Rheumatoid Arthritis Disease?
- Treating rheumatoid arthritis to target: recommendations of an international task force
- Incorporating the Treat-to-Target Concept in Rheumatoid Arthritis
- Effect of a treatment strategy of tight control for rheumatoid arthritis (the TICORA study): a single-blind randomised controlled trial
INDEX OF TOPICS
Introduction
1. Fundamentals of care in RD
2. Care management
3. Pain control
4. Patient reported outcome measures
5. Collaboration among physicians
6. Knowledge of RD
7. Use of imaging
8. Patient symptoms
9. Referrals suited to risk
10. Treat to target
FOOTNOTES FOR GOOD CARE TOOLBOX
1 Pincus, T. The science of MDHAQ/RAPID3 scores: Do patient self-reports provide valid data for evidence-based care in rheumatology practice? 2011 Dec [cited 2013 Aug 2]. The Rheumatologist. Available from: http://www.the-rheumatologist.org/details/article/1421273/The_Science_of_MDHAQRAPID3_Scores.html
2 Kremers HM, Bidaut-Russell M, Scott CG, Reinalda MS, Zinsmeister AR, Gabriel SE. Preventive medical services among patients with rheumatoid arthritis. J Rheumatol. 2003 Sep [PDF accessed 2010 Aug 19 and Abstract accessed 2013 Feb 20];30(9):1940-1947. Available from: http://www.jrheum.org/content/30/9/1940.abstract
3 Desai SS, Myles JD, Kaplan MJ. Suboptimal cardiovascular risk factor identification and management in patients with rheumatoid arthritis: a cohort analysis. Ann rheum dis. 2012 Dec [cited 2013 Feb 20]; 14:R270. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19773290
4 Young, K. Why rheumatoid disease patients still fall through the cracks. Rheumatoid Arthritis Warrior [website]. 2013 Feb 13 [cited 2013 Aug 2]. Available from: https://www.rawarrior.com/why-rheumatoid-disease-patients-still-fall-through-the-cracks/
5 American College of Rheumatology. Position statement: The rheumatologist as principal care physician. 2011 Aug [cited 2013 Aug 2]. Available from: http://www.rheumatology.org/practice/clinical/position/rheumatologistPrincipalCare.pdf
6 Holmes, C. The problem list beyond meaningful use. Journal of AHIMA [website]. 2011 Apr 6 [cited 2013 Aug 2] Available from: http://journal.ahima.org/2011/04/06/the-problem-list-beyond-meaningful-use/
7 Harrold LR, Harrington JT, Curtis JR, Furst DE, Bentley MJ, Shan Y, Reed G, Kremer J, Greenberg JD. Prescribing practices in a US cohort of rheumatoid arthritis patients before and after publication of the American College of Rheumatology treatment recommendations. Arthritis & Rheumatism. 2012 Mar [cited 2013 Aug 2];64(3):630–638. Available from: http://onlinelibrary.wiley.com/doi/10.1002/art.33380/full
8 Hmamouchi I, Bahiri R, Srifi N, Aktaou S, Abouqal R, Hajjaj-Hassouni N. A comparison of ultrasound and clinical examination in the detection of flexor tenosynovitis in early arthritis. BMC Musculoskeletal Disorders. 2011 [cited 2013 Aug 3];12:91. Available from: http://www.biomedcentral.com/1471-2474/12/91
9 Aletaha D, Funovits J, Smolen JS. Physical disability in rheumatoid arthritis is associated with cartilage damage rather than bone destruction. Ann Rheum Dis 2011 [cited 2013 Aug 3];70:733-739. Available from: http://ard.bmj.com/content/70/5/733.full
10 Brown AK, Quinn MA, Karim Z, Conaghan PG, Peterfy CG, Hensor E, Wakefield RJ, O’Connor PJ, Emery P. Presence of significant synovitis in rheumatoid arthritis patients with disease-modifying antirheumatic drug–induced clinical remission: Evidence from an imaging study may explain structural progression. Arthritis Rheum. 2006 Dec [cited 2013 Aug 3];54(12):3761–3773. Available from: http://onlinelibrary.wiley.com/store/10.1002/art.22190/asset/22190_ftp.pdf?v=1&t=hjwu6cbq&s=a90ec1f341093085e7bb0dcffdf8e1d5cf8179c7
11 McAlindon T, Kissin E, Nazarian L, Ranganath V, Prakash S, Taylor M, Bannuru RR, Srinivasan S, Gogia M, McMahon MA, Grossman J, Kafaja S, FitzGerald J. American College of Rheumatology report on reasonable use of musculoskeletal ultrasonography in rheumatology clinical practice. Arthritis Care Res. 2012 Nov [cited 2013 Aug 3];64(11): 1625–1640. Available from: http://onlinelibrary.wiley.com/doi/10.1002/acr.21836/full
12 Colebatch AN, Edwards CJ, Østergaard M, van der Heijde D, Balint PV, D’Agostino MA, Forslind K, Grassi W, Haavardsholm EA, Haugeberg G, et al. EULAR recommendations for the use of imaging of the joints in the clinical management of rheumatoid arthritis. Ann Rheum Dis. 2013 Mar 21 [cited 2013 Aug 3]; Recommendation. Available from: http://ard.bmj.com/content/early/2013/03/20/annrheumdis-2012-203158.full
13 Zoler ML. Ultrasound speeds new RA diagnoses. Rheumatology News [website]. 2013 Jul 11 [cited 2013 Aug 3]. Available from: http://www.rheumatologynews.com/specialty-focus/rheumatoid-arthritis/single-article-page/ultrasound-speeds-new-ra-diagnoses/
14 Adams RF. An identity crisis for RA: a few suggestions to bring rheumatic disease the recognition and respect it deserves [Internet]. Atlanta (GA): American College of Rheumatology. The Rheumatologist; 2011 Aug 14 [cited 2013 Aug 3]. Available from: http://www.the-rheumatologist.org/details/article/1311755/An_Identity_Crisis_for_RA.html
15 Strand V, Emery P, Fleming S, Griffin C. The impact of rheumatoid arthritis (RA) on women: focus on pain, productivity and relationships [abstract]. Arthritis Rheum [Internet]. 2010 [cited 2013 Aug 3];62 Suppl 10:1063. Available from: http://www.blackwellpublishing.com/acrmeeting/abstract.asp?MeetingID=774&id=89712
16 Rheumatoid Patient Foundation. Unmasking rheumatoid disease: the patient experience of rheumatoid arthritis. A white paper from the Rheumatoid Patient Foundation. Rheumatoid Patient Foundation [Internet]. 2013 Apr 20 [cited 2013 Aug 3]. Available from: http://rheum4us.org/wp-content/uploads/2013/04/Unmasking-Rheumatoid-Disease-The-Patient-Experience-of-Rheumatoid-Arthritis-White-Paper.pdf
17 Mayo Clinic. Rheumatoid arthritis patients at higher risk for unrecognized heart disease. Newswise [website]. 2005 Feb 1 [cited 2013 Aug 3]. Available from: http://www.newswise.com/articles/view/509590/
18 Whitmore M. Living with a spouse with chronic illness, part 2. Rheumatoid Arthritis Warrior [website]. 2010 Jul 2 [cited 2013 Aug 3]. Available from: https://www.rawarrior.com/living-with-a-spouse-with-chronic-illness-part-2/
19 Ruderman EM, Nola KM, Ferrell S, Sapir T, Cameron DR. Incorporating the treat-to-target concept in rheumatoid arthritis. J Manag Care Pharm. 2012 Nov-Dec;18(9):1-18
20 Vermeer M, Kuper HH, Moens HJB, Drossaers-Bakker KW, van der Bijl AE, van Riel PLCM, van de Laar MAFJ. Sustained beneficial effects of a protocolized treat-to-target strategy in very early rheumatoid arthritis: Three-year results of the Dutch rheumatoid arthritis monitoring remission induction cohort. Arthrit Care Res. 2013 Jul 26 [cited 2013 Aug 8];5(8):pages 1219–1226. Available from: http://onlinelibrary.wiley.com/doi/10.1002/acr.21984/abstract
21 Grigor C, Capell H, Stirling A, et al. Effect of a treatment strategy of tight control for rheumatoid arthritis (the TICORA study): a single-blind randomised controlled trial. Lancet. 2004;364:263-269
22 Smolen JS, Aletaha D, Bijlsma JW, et al. Treating rheumatoid arthritis to target: recommendations of an international task force [published correction appears in Ann Rheum Dis. 2011;70:1519]. Ann Rheum Dis. 2010;69:631-637



